- ONCOLOGY Vol 14 No 9
- Volume 14
- Issue 9
Recent Developments in Chemoradiotherapy for Locally Advanced Cancer of the Cervix
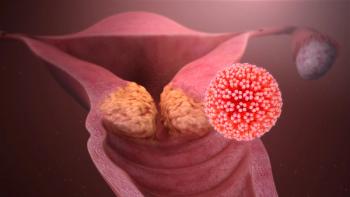
Patients with locally advanced cervical cancer comprise a significant proportion of the total population with cervical cancer, particularly in developing countries. The inability to control pelvic tumors is still a significant
Drs. Kim and Alvarez have written an excellent, in-depth review and update on the use of chemotherapy as an adjunct to radiation therapy in locally advanced cervical cancer, elegantly summarizing recent study results. New evidence of the benefits of adjuvant chemotherapy[1-5] has been, by far, the most significant breakthrough of the past several decades in the treatment of women with this disease.
In their article, the authors convincingly show that chemotherapy must be given concurrently with, not before, radiation therapy in order to be effective. They summarize the disappointing outcomes of neoadjuvant chemotherapy studies and provide radiobiological rationales for the observed clinical resultslimited tumor response rate to chemotherapy alone, accelerated repopulation, and therapy delayexplanations that, in retrospect, seem logical.
Concurrent Radiosensitizing Chemotherapy
The concurrent use of cytotoxic and radiosensitizing drugs with radiation therapy improves survival in advanced cervical cancer by 15% (P = .004)[1], over radiotherapy alone, a gain that had not been achieved by altered fractionation, hyperbaric oxygen or previous radiosensitizers (eg, hydroxyurea). These recent studies have now reproduced the favorable results of concurrent cisplatin (Platinol)-based radiosensitizing chemotherapy in epithelial head and neck, esophageal, and anal cancer and demonstrated that the use of radiosensitizing cytotoxic agents can produce clinically relevant modulation of radiotherapy outcome in yet another epithelial tumor: cervical cancer.
The authors suggest, however, that the promising results of these studies leave us with more questions than answers: Which concurrent chemotherapy regimen is optimal? Which regimens are appropriate for which patients?
Which Combination to Choose?
Choosing the optimal concurrent chemotherapy combination in patients treated with radiation therapy for advanced cervical cancer remains a challenge. Only one study has randomized patients with nonresected disease to a control arm of radiation therapy alone vs cisplatin-based chemoradiotherapy.[1] In this trial, the two-drug combination of cisplatin and fluorouracil (5-FU) improved pelvic tumor control and survival. Based on these data, should cisplatin/5-FU become the standard adjunct for patients treated with radiation therapy for advanced disease? The answer is clearly controversial.
Gynecologic Oncology Group (GOG) study 120[3] randomized the triple-drug combination cisplatin/5-FU/hydroxyurea vs cisplatin alone in slightly different patient populations (surgically staged, node-negative patients). Comparison of one vs three radiosensitizers showed no advantage over the single-agent cisplatin regimen. However, the confounding factor of hydroxyurea, which has since been shown to be ineffective and to increase toxicity, makes these results difficult to interpret.[6,7]
Would two effective radiosensitizers be better than one? A randomized comparison of one vs two well-established cytotoxic radiosensitizersie, cisplatin vs cisplatin/5-FUhas yet to be conducted, and there are presently no plans for such a comparison in cooperative groups. However, the ongoing GOG study 165 is comparing cisplatin and 5-FU as single-agent adjuncts to radiation therapy.
Meanwhile, new cytotoxic and radiosensitizing agents are being developed and entering clinical trials. Paclitaxel (Taxol), which has radiosensitizing properties,[8] is being studied in phase I trials as an adjunct to radiation therapy.[9] The topoisomerase inhibitor topotecan (Hycamtin), may be another candidate for concurrent use with radiation therapy.[10,11]
With the impending availability of several chemotherapy agents for concurrent use with radiation therapy, the next question will be how to optimally select, combine, and time these agents with radiation therapy in order to maximize responseparticularly in patients who remain at high risk for treatment failure, despite presently used concurrent chemoradiation therapy regimens.[1,2]
Better Staging and Outcome Predictors
How can we determine the appropriate degree of (local and/or systemic) therapy intensity for the individual patient, in order to provide the best chance of tumor control and least chance of morbidity for her particular tumor, and at what risk? Do we have sufficient outcome predictors to categorize tumor aggressiveness and help determine therapy selection?
The classic staging evaluations and the International Federation of Gynecology and Obstetrics (FIGO) staging system, upon which entry into the recent randomized studies[1-5] was largely based, have been widely criticized as suboptimal in determining the true extent of the primary tumor, regional extension, and biological aggressiveness of cervical cancer. We need to develop a refined prognostic algorithm of tumor aggressiveness beyond clinically/radiographically based staging to determine the intensity of required therapy.
Tumor-cell hypoxia and tumor blood supply remain among the most important biological parameters of radiation response; they may also relate to chemotherapy response and metastatic potential.[12-14] However, assays available to the clinic to assess these factors have been difficult to implement in the patient care setting, requiring, for example, insertion of needle oximetry electrodes for hypoxia measurements[13] or other invasive procedures.
The recent advances, increasing availability, and decreasing cost of tumor-imaging modalities provide new opportunities to refine staging and therapy outcome prediction. Functional tumor imaging, such as magnetic resonance perfusion imaging,[15] have made the assessment of microvascular function and tumor microcirculation (which is closely related to tumor hypoxia) easier to accomplish in day-to-day clinical practice and widely available for patient management.
Beyond these imaging-based parameters, new molecular predictors of therapeutic response are also emerging. Molecular predictors, including the mitotic index of proliferating cells, Ki-67, HER2, bcl-2, and BAX, have been shown to predict response to radiation therapy and may be useful prognostic markers.[16-19] These novel outcome predictors hold promise in providing us with parameters of tumor aggressiveness that can be feasibly employed in daily clinical practice. They may provide guidance for the selection of therapy intensity, particularly with respect to multimodality therapy and adjuvant chemotherapy.[20]
Increased Morbidity vs Survival Benefits
It is likely that the addition of chemotherapy to radiation therapy will increase treatment-related morbidity. Although short-term hematologic and gastrointestinal toxicities are relatively easy to overcome, long-term therapy-related complications in the bowel and other pelvic organs as well as second malignancies[21] are of greater concern. It will take at least another decade of follow-up data from the randomized studies to quantify the risk of late morbidity. In the interim, radiation oncologists must make a maximal effort to reduce this risk.
Recent advances in radiation therapy techniques, including three-dimensional, imaging-based radiotherapy planning, provide an opportunity to further reduce the volume of normal tissues, particularly the bowel, in the treatment field for external-beam radiation. By implementing imaging-based, and where applicable, conformal radiation therapy, and perhaps by using a more conformal imaging-based approach for brachytherapy, we may be able to further reduce the probability of complications in normal tissues. Cytoprotective agents, such as amifostine (Ethyol), may also supplement these efforts to reduce toxicity[22] and should be fully explored.
Conclusions
We have never had more options at hand in the therapy of women with advanced cervical cancerconcurrent chemotherapy, emerging functional/biological outcome predictors, high-precision imaging-based radiation therapy, and cytoprotective agents. The challenge of the next decade will be to employ these tools wisely so that not only the tumor response, but also the lives of women with advanced cervical cancer, can be improved.
References:
1. Morris M, Eifel PJ, Lu J, et al: Pelvic radiation with concurrent chemotherapy with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340:1137-1143, 1999.
2. Whitney CW, Sause W, Bundy BN, et al: Randomized comparison of fluorouracil plus cisplatin vs hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: A Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol 17:1339-1348, 1999.
3. Rose PG, Bundy BN, Watkins EB, et al: Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 340:1144-1153, 1999.
4. Peters WA III, Liu PY, Barrett R, et al: Cisplatin, 5-fluorouracil plus radiation therapy are superior to radiation therapy as adjunctive in high-risk, early-stage carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy (abstract). Gynecol Oncol 72:443, 1999.
5. Keys HM, Bundy BN, Stehman FB, et al: Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med 340:1154-1161, 1999.
6. Stehman FB, Bundy BN, Keys H, et al: A randomized trial of hydroxyurea vs misonidazole adjunct to radiation therapy in carcinoma of the cervix: A preliminary report of a Gynecologic Oncology Group study. Am J Obstet Gynecol 159:87-94, 1988.
7. Leibel S, Bauer M, Wasserman T, et al: Radiotherapy with or without misonidazole for patients with stage IIIB or IVA squamous cell carcinoma of the uterine cervix: Preliminary report of a Radiation Therapy Oncology Group randomized trial. Int J Radiat Oncol Biol Phys 13:541-549, 1987.
8. Liebmann J, Cook JA, Fisher J, et al: In vitro studies of Taxol as a radiation sensitizer in human tumor cells. J Natl Cancer Inst 86:441-446, 1994.
9. Chen MD, Paley PJ, Potish RA, et al: Phase I trial of Taxol as a radiation sensitizer with cisplatin in advanced cervical cancer. Gynecol Oncol 67:131-136, 1997.
10. Lamond JP, Wang M, Kinsella TJ, et al: Concentration and timing dependence of lethality enhancement between topotecan, a topoisomerase I inhibitor, and ionizing radiation. Int J Radiat Oncol Biol Phys 36:361-368, 1996.
11. Rich TA, Kirichenko AV: Camptothecin radiation sensitization: Mechanisms, schedules, and timing. Oncology 12(suppl 6):114-120, 1998.
12. Brizel DM, Scully SP, Harrelson JM, et al: Tumor oxygenation predicts for likelihood of distant metastases in human soft tissue sarcoma. Cancer Res 46:941-943, 1996.
13. Höckel M, Schlenger K, Aral B, et al: Association between tumor hypoxia and malignant progression in advanced cancer of the uterine cervix. Cancer Res 56:4509-4515, 1996.
14. Hawighorst H, Knapstein P, Weikel W, et al: Angiogenesis of uterine cervical carcinoma: Characterization by pharmacokinetic magnetic resonance imaging-based parameters and a histomorphological approach in correlation with disease outcome. Clin Cancer Res 4:2305-2312, 1998.
15. Mayr NA, Hawighorst H, Yuh WTC, et al: MR microcirculation in cervical cancer: Correlations with histomorphological tumor markers and clinical outcome. J Magn Reson Imaging 10:267-276, 1999.
16. Pillai MR, Jayaprakash PG, Nair MK: Bcl-2 immunoreactivity but not p53 accumulation associated with tumour response to radiotherapy in cervical carcinoma. J Cancer Res Clin Oncol 125(1):55-60, 1999.
17. Harima Y, Harima K, Shikata N, et al: Bax and Bcl-2 expressions predict response to radiotherapy in human cervical cancer. J Cancer Res Clin Oncol 124(9):503-510, 1998.
18. Nakano T, Oka K: Differential values of Ki-67 index and mitotic index of proliferating cell population: An assessment of cell cycle and prognosis in radiation therapy for cervical cancer. Cancer 72(8):2401-2408, 1993.
19. Nakano T, Oka K, Ishikawa A, et al: Immunohistochemical prediction of radiation response and local control in radiation therapy for cervical cancer. Cancer Detect Prev 22(2):120-128, 1998.
20. Mayr NA, Yuh WTC, Magnotta VA, et al: Tumor perfusion studies using fast magnetic resonance imaging technique in advanced cervical cancer: A new noninvasive predictive assay. Int J Radiat Oncol Biol Phys 36:623-633, 1996.
21. Travis LB, Holowaty EJ, Bergfeldt K, et al: Risk of leukemia after platinum-based chemotherapy for ovarian cancer. N Engl J Med 340(5):351-357, 1999.
22. Altmann S, Hoffmanns H: Cytoprotection with amifostine in radiotherapy or radio-chemotherapy of head and neck tumors [German]. Strahlenther Onkol 175(suppl 4):30-33, 1999.
Articles in this issue
over 25 years ago
Cancer Treatment Billover 25 years ago
Optimal Use of the Newer Antifungal Agentsover 25 years ago
New Awards Spotlight Courage of Cancer Survivorsover 25 years ago
Hematopoietic Cell Transplantation, Second Editionover 25 years ago
ASCO to Push Medicare on Fee Issueover 25 years ago
Tamoxifen Approved for Use in Patients With Ductal Carcinoma In Situover 25 years ago
IG Guidelines on Individual Physicians and Small PracticesNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.