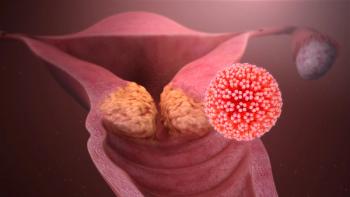
Self-Samples as Effective as Clinician Samples for HPV Screening?
A study investigates whether HPV testing performed on cervicovaginal samples self-collected by patients had a similar accuracy to samples collected by clinicians.
HPV testing performed on cervicovaginal samples self-collected by patients had a similar accuracy for identifying cervical intraepithelial neoplasia (CIN) as samples collected by clinicians, according to the results of the IMPROVE study published in Lancet Oncology.
“These
More than 180,000 women were invited to participate in the IMPROVE study, which was designed to assess the accuracy of primary HPV testing done using self-collected samples. Of these, 7,643 women were randomly assigned to the self-sampling group and 6,282 to the clinician-based sampling group.
According to the study, use of self-sampling for HPV screening is expected to reduce the cost of screening and the workload of clinicians.
“In the Netherlands, about 500,000 cervical samples are taken annually,” the researchers wrote. “We expect a reduction of at least 90% by HPV self-sampling because only HPV-positive women require cervical sampling by a clinician.”
However, the researchers also acknowledged that cost of screening will depend on the HPV self-sampling device, which can be priced higher than brushes used by clinicians.
For self-sampling, women were asked to collect their own cervicovaginal sample using an Evalyn Brush.
“The Evalyn Brush is designed for HPV self-sampling, including wings indicating the depth of insertion and audible clicks for counting the number of rotations,” the researchers wrote.
A Cervex-Brush was used by clinicians. All samples from both groups were tested for HPV using the GP5+/6+ PCR enzyme immunoassay.
About 7% of samples tested positive for HPV in both groups (7.4% in self-collected and 7.2% in clinician-collected samples).There was a slightly higher sample of under-screened women in the self-sampling group compared with the clinician group (13% vs 7%).
The sensitivity and specificity for detecting was similar between the two groups for both CIN2+ (relative sensitivity, 0.96; relative specificity, 1.00) and CIN3+ (relative sensitivity, 0.99; relative specificity, 1.00).
Based on these results, the researchers wrote that “HPV self-sampling has potential for use as a primary screening test, but its clinical accuracy needs to be established with a high level of confidence.”
According to an editorial published with the study written by Elsebeth Lynge, PhD, of the University of Copenhagen, Denmark, the technical specifications used should be considered in the interpretation of the results.
“In the 2014 meta-analysis, no difference was found between sample types in terms of sensitivity for CIN2+ in the few studies that used the GP5+/6+ PCR assay for HPV testing, and the overall reduced sensitivity of the self-collected samples was driven by results from studies that used the Hybrid Capture 2 assay for HPV testing,” Lynge wrote. “Further comparisons between outcomes of the GP5+/6+ PCR assay with those of new generation HPV assays are therefore needed before conversion to self-collection can be generally considered in screening programmes.”
Commenting on the study results, Marc Arbyn, MD, MSc, PhD, told Cancer Network, "The findings are completely in line with a recent systematic review (Arbyn, BMJ, December 2018) showing that hrHPV DNA testing on self- and clinician samples have similar accuracy for detecting cervical precancer under the condition that a clinically validated PCR assay is used. HPV-based screening on self-samples offers opportunities to increase population coverage. Self-sampling strategies are more effective to reach women who do not attend routine screening than invitations to have a specimen taken in a clinic."
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.