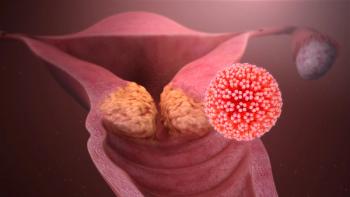
Using Any HPV Vaccination May Reduce Burden of Disease
Researchers suggested that the receipt of 1, 2, or 3 doses of an HPV vaccine by females aged 15 to 19 years was associated with a lower incidence of preinvasive cervical disease when compared to unvaccinated females.
In a database study published in Cancer, the receipt of 1, 2, or 3 doses of an HPV vaccine by females aged 15-19 years was associated with a lower incidence of preinvasive cervical disease in comparison with unvaccinated females.1
These data support the use of any HPV vaccination in reducing the burden of this disease.
“HPV-related disease remains a significant source of morbidity and mortality in both developed and developing countries, and this underscores the need to increase vaccination coverage to effectively reduce HPV infection and disease,” the authors wrote.
Using Optum’s Clinformatics DataMart Database to identify females aged 9-26 years who received 1 or more quadrivalent HPV vaccine doses between January 2006 and June 2015, researchers matched 66,541 vaccinated females to 66,541 unvaccinated females based on region, age, sexually transmitted disease history, and pregnancy. The participants were stratified based on the number of HPV vaccine doses and the vaccine initiation age.
Of those aged 15-19 years, the hazard ratio (HR) for high-grade cytology for the 3-dose group was 0.84 (95% CI, 0.47-0.88), whereas the HRs for histologically confirmed preinvasive cervical disease for 1, 2, and 3 doses were 0.64 (95% CI, 0.47-0.88), 0.72 (95% CI, 0.54-0.95), and 0.66 (95% CI, 0.55-0.80), respectively.
“Current evidence clearly indicates that vaccinating younger individuals is more effective,” the authors wrote. “The average age of first sexual intercourse for US females is 16-18 years. The vaccine is more efficacious in HPV-naïve cohorts, and the immune response is more robust, especially in adolescent females younger than 15 years.”
Notably, the information used for outcome analysis came from diagnosis codes and relied on insurance claims for outpatient and hospitalization services, which the researchers indicated are not always accurate or complete. Additionally, the authors suggested that the database lacked information on factors that may influence the risk of preinvasive cervical disease or compliance with HPV testing or screening, such as race/ethnicity, socioeconomic or other demographic factors, sexual history, and family history of cancer.
“Future studies are needed to examine screening behaviors among those vaccinated at later ages,” the authors wrote. “More long-term follow-up data are needed to draw definitive conclusions.”
In an editorial written by Julia M. L. Brotherton, MPH, PhD, from the VCS Foundation, and Karin Sundström, MD, PhD, from the Karolinska Institutet, suggested that this data gives the 1-dose effectiveness hypothesis further credibility.2
“If 1 dose of an HPV vaccine were sufficient for effective protection, HPV vaccine implementation and scale-up would require less logistics (while being amenable to a periodic campaign approach), available doses could be extended further, and the overall cost would be lower,” the editorial authors wrote. “In summary, these data add to the growing evidence suggesting that there may truly be no major difference in protection against cervical preinvasive lesions, up to 10 years so far, conferred by 1, 2, or 3 doses of HPV vaccination.
References:
1. Rodriguez AM, Zeybek B, Vaughn M, et al. Comparison of the Long-Term Impact and Clinical Outcomes of Fewer Doses and Standard Doses of Human Papillomavirus Vaccine in the United States: A Database Study. Cancer. doi:10.1002/cncr.32700.
2. Brotherton JML, Sundtröm K. More Evidence Suggesting that 1-Dose Human Papillomavirus Vaccination May Be Effective. Cancer. doi:10.1002/cncr.32696.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.