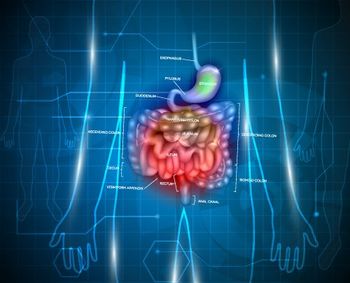
What Is Required for Accurate Lymph Node Staging in Small-Bowel NETs?
Among patients with small-bowel neuroendocrine tumors, accurate lymph node staging may require the examination of at least eight lymph nodes.
Among patients with small-bowel neuroendocrine tumors (SB-NETs), accurate lymph node staging may require the examination of at least eight lymph nodes, according to a new study. The presence of at least four positive lymph nodes was associated with decreased recurrence-free survival (RFS).
In other malignancies, surgical resection of tumor-draining lymph nodes has been questioned, since extensive lymph node dissection can be associated with substantial morbidity, but in SB-NETs, regional lymphadenectomy has been associated with improved survival. “Nonetheless, the extent of lymphadenectomy has come under question,” wrote study authors led by Mohammad Y. Zaidi, MD, MS, of the
The number of lymph nodes needed to stage accurately was not well understood, so the authors conducted a study using information from a database maintained by the US Neuroendocrine Tumor Study Group. They included a total of 199 patients who underwent resection with curative intent of SB-NETs between 2000 and 2015; the results of the analysis were
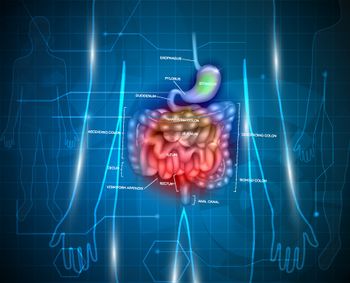
The mean age of patients in the study was 60.3 years, and 56.3% were male. Most patients were white (76.4%), and the mean BMI was 29.5. The mean tumor size was 2.2 cm, and 91.4% were well-differentiated tumors. Most patients (69.5%) had lymphovascular invasion. The median number of lymph nodes retrieved was 13, and 77.4% were lymph node positive; the median number of positive lymph nodes was 3.
Patients were followed for a median of 39 months, and the median RFS was not reached. Thirty-two patients had disease recurrence (16.1%); of those, 28.1% were local recurrences, 68.8% were distant recurrences, and 1 patient (3.1%) had both a local and a distant recurrence.
No association with a reduced RFS was seen among patients with 1; 1 to 2; 2; or 2 to 3 positive lymph nodes compared with patients with lymph node–negative disease. Once the threshold of 4 positive nodes was crossed, however, an association did emerge; those patients had a worse 3-year RFS compared with those with 1 to 3 positive nodes and those with negative lymph nodes (81.6%, 91.4%, and 92.1%, respectively; P = .01). A multivariate analysis showed that 4 or more positive lymph nodes was associated with decreased RFS, with a hazard ratio of 3.03 (95% CI, 1.30–7.06; P = .01).
Retrieving 8 or more lymph nodes appeared to be important for accurate staging. In patients who had fewer than 8 lymph nodes resected, there was no difference in 3-year RFS between those with 4 or more positive nodes and those with fewer or no positive nodes (P = .87). In those with 8 or more lymph nodes resected, those differences did emerge (P = .05).
“Accurate staging of these patients requires a minimum of 8 lymph nodes for examination,” the authors concluded. “Complete regional lymphadenectomy may need to be performed routinely.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.