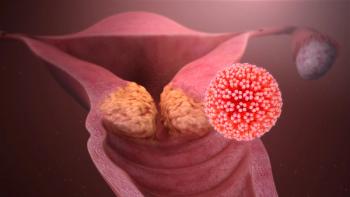
WHO Strategy Could Help to Reduce Cervical Cancer Mortality
If successfully implemented, researchers found that over the next century, cervical cancer mortality would be reduced by almost 99% and save more than 62 million women’s lives.
According to an article published in The Lancet, over the next 10 years, a one-third reduction in the rate of premature mortality from cervical cancer in low-income and lower-middle-income countries is possible, contributing to the realization of the 2030 UN Sustainable Development Goals.
Over the next century, the researchers indicated that successful implementation of the World Health Organization (WHO) elimination strategy would reduce cervical cancer mortality by almost 99% and save more than 62 million women’s lives.
The data presented will help inform the draft WHO global strategy for cervical cancer elimination, which will be presented to the WHO Executive Board in February 2020 and then later considered at the World Health Assembly in May 2020.
“The key will be the effective implementation of all 3 of the strategies (vaccination, screening and cancer treatment) in all countries including low income countries, and also in disadvantaged groups within higher income country populations. New technology is a part of the answer because it helps open up new models of delivery for the key interventions,” said Karen Canfell, PhD, director of the cancer research division at the Cancer Council NSW. “Ultimately women themselves, in each community, need to be at the center of the elimination initiative.”
Using the WHO Cervical Cancer Elimination Modelling Consortium (CCEMC) researchers projected reductions in age-standardized rates of cervical cancer mortality in 78 low-income and lower-middle-income countries for three standardized base-case scenarios, including girls-only vaccination at age 9 years with catch-up for girls aged 10-14 years, girls-only vaccination plus once-lifetime screening and cancer treatment scale-up, and girls-only vaccination plus twice-lifetime screening and cancer treatment scale-up.
In 2020, the estimated cervical cancer mortality rate across all 78 low-income and lower-middle-income countries was 13.2 (range, 12.9-14.1) per 100,000 women. Comparatively, by 2030, researchers suggested that vaccination alone would have minimal impact on cervical cancer mortality, leading to a 0.1% (range, 0.1%-0.5%) reduction; however by also scaling up twice-lifetime screening and cancer treatment, mortality rates would be reduced by 34.2% (range, 23.3%-37.8%), averting 300,000 (range, 300,000-400,000) deaths by 2030 (with similar results shown for once-lifetime screening).
Moreover, by 2070, scaling up vaccination alone could reduce mortality by 61.7% (range, 61.4%-66.1%), averting 4.8 million (range, 4.1-4.8 million) deaths. In additionally scaling up screening and cancer treatment, by 2070 there could be a reduction in mortality by 88.9% (range, 84.0%-89.3%), averting 13.3 million (range, 13.1-13.6 million) deaths (with once-lifetime screening), or by 92.3% (range, 88.4%-93.0%), averting 14.6 million (range, 14.1-14.6 million) deaths (with twice-lifetime screening).
Furthermore, by 2120, vaccination alone could reduce mortality by 89.5% (range, 86.6%-89.9%), averting 45.8 million (range, 44.7-46.4 deaths). By scaling up screening and cancer treatment, by 2120 researchers observed an additional reduction in mortality of 97.9% (range, 95.0%-98.0%), averting 60.8 million (range, 60.2-61.2 million) deaths (with once-lifetime screening), or by 98.6% (range, 96.5%-98.6%), averting 62.6 million (range, 62.1-62.8 million) deaths (with twice-lifetime screening).
“I think the key value of these findings is that it helps all stakeholders to understand how the different interventions across the cancer control spectrum – vaccination, cervical screening, and cervical cancer treatment – will interact with each other and how the timing of their joint effects will support both early impact and longer term efforts to achieve elimination,” Canfell explained.
Utilizing the WHO triple-intervention strategy over the next 10 years, about half (48%; range, 45.0%-55.0%) of deaths averted would be in sub-Saharan Africa and almost a third (32%; range, 29%-34%) would be in South Asia. Additionally, over the next 100 years, almost 90% of deaths averted would be in these regions as well. In regard to premature deaths (age 30-69 years), the WHO triple intervention strategy would result in rate reductions of 33.9% (range, 24.4%-37.9%) by 2030, 96.2% (range, 94.3%-96.8%) by 2070, and 98.6% (range, 96.9%-98.9%) by 2120.
Implementation of this elimination initiative could afford the opportunity for both nearer-term and enduring positive consequences, not only for women in general, but also for their families and society as a whole.
“As researchers, we have all come together to work towards supporting WHO and its partners in the strategic planning for cervical cancer elimination,” said Canfell. “That is what makes this work so exciting for us.”
Reference:
Canfell K, Kim JJ, Brisson M, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. The Lancet. doi:10.1016/S0140-6736(20)30157-4.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.