- Oncology Vol 29 No 10
- Volume 29
- Issue 10
Axillary Surgery After Chemotherapy: Challenges and Opportunities
While breast-conserving surgery after neoadjuvant chemotherapy has become more accepted over time, methods of management of the axillary lymph nodes have remained matters of controversy.
The approach to management of breast cancer patients has evolved from one of primary surgical treatment, in which traditional TNM staging dictated the need for adjuvant therapy, to a multidisciplinary one, with sequencing of surgical and systemic therapy determined by the biologic subtype of each tumor. Two decades ago, chemotherapy was administered preoperatively (neoadjuvant chemotherapy) to patients with locally advanced breast cancer, both to initiate early treatment of systemic disease and to convert inoperable disease to an operable status. Early trials demonstrated that neoadjuvant chemotherapy could be administered safely to patients with locally advanced disease without losing the surgical window of opportunity[1]; trials also showed that some patients had significant reduction in tumor burden with neoadjuvant chemotherapy, thereby allowing for breast-conserving surgery.[2]
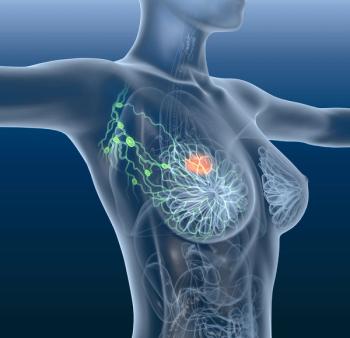
Patients who achieve a pathologic complete response (pCR) to neoadjuvant chemotherapy have more favorable outcomes, and nodal status after chemotherapy is a strong prognostic indicator of survival.[3,4] As systemic treatment regimens have evolved from a one-size-fits-all approach to a more targeted one based on underlying tumor biology, response rates in the primary tumor and regional nodal basins have increased, as has the likelihood of achieving pCR.[5] While breast-conserving surgery after neoadjuvant chemotherapy has become more accepted over time, methods of management of the axillary lymph nodes have remained matters of controversy.
In this issue of ONCOLOGY, Manguso et al review the published literature on the use of sentinel lymph node biopsy (SLNB) in patients receiving neoadjuvant chemotherapy; they conclude that while some patients may be able to avoid axillary lymph node dissection (ALND), those who are node-positive prior to chemotherapy should still undergo ALND after chemotherapy.[6] While on the surface, this may seem like a reasonable assumption, a deeper dive into the available data may lead to a different conclusion.
The majority of the literature on the use of SLNB after neoadjuvant chemotherapy comes from single-institution reports of retrospective data. Although this type of data can be hypothesis-generating, it is unlikely to provide robust support that can be used to change clinical practice. Several meta-analyses have attempted to combine single-institution data with the limited multi-institution data that are available, and the majority have concluded that SLNB is accurate after chemotherapy.[7-10] These analyses included studies that did not clearly define nodal status prior to chemotherapy, and some included both clinically node-negative and clinically node-positive patients. Very few studies evaluated response in the nodal basin prior to surgery, and many different surgical approaches were employed (eg, blue dye alone, isotope alone, combination blue dye and isotope). Studies of SLNB in both the upfront surgery and the post–neoadjuvant chemotherapy settings have reported higher identification rates and lower false-negative rates with SLNB performed with a combination of blue dye and isotope, and the number of sentinel lymph nodes removed has been shown to have significant impact on the false-negative rate.[11] Research at MD Anderson Cancer Center has shown that in patients with initially clinically node-negative disease, SLNB after neoadjuvant chemotherapy is just as accurate as in the upfront surgery setting.[12] In addition, in patients with initially clinically node-negative disease, SLNB after neoadjuvant chemotherapy eradicates occult nodal disease in a proportion of patients, eliminating the need for ALND in some patients and providing important prognostic information based on the presence or absence of nodal disease following chemotherapy.
While it has been standard at MD Anderson to use ultrasound prior to chemotherapy to evaluate regional nodal basins, computed tomography and positron emission tomography scans, which are suggested by Manguso et al, were not routinely performed. In a recent study of patients who received neoadjuvant chemotherapy compared with those who underwent surgery first, patients who underwent upfront surgery had an increased likelihood of positive sentinel lymph nodes with increasing T stage.[12] Similar to results in other institutional reports, a reduced incidence of node-positive disease (by T stage, in comparison with patients undergoing upfront surgery) was also seen in patients undergoing neoadjuvant chemotherapy. Findings from the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-18 and B-27 randomized trials and the European Organisation for Research and Treatment of Cancer (EORTC) 10902 trial have also demonstrated this nodal downstaging.[13-15]
Until recently, data on the use of SLNB after chemotherapy in patients with initially node-positive disease also came largely from retrospective, single-institution studies. Manguso et al discuss several multicenter trials that have now reported outcomes in this patient population.[11,16,17] Interestingly, all reported higher identification rates and lower false-negative rates than the single-institution reports, but with false-negative rates as high as 14%,[11,16,17] the applicability of SLNB in this setting has come into question. Several important points should be considered, however, when examining these trial results. One is that not all of the studies required biopsy confirmation of nodal status prior to chemotherapy. We now know, though, that relying on physical examination to define nodal status is likely to lead to inaccurate staging in a substantial proportion of patients. Second, response to chemotherapy was not used to select patients for SLNB after chemotherapy. This means that patients with significant residual disease in the axilla were included and may have contributed to higher false-negative rates. Finally, there was no attempt to mark and remove the axillary node that was biopsied at presentation in order to confirm removal of the index node at the time of surgery. In the American College of Surgeons Oncology Group (ACOSOG) Z1071 trial,[11] it was reported that when a clip was placed at the time of initial node biopsy and the clipped node was confirmed to be removed with SLNB, the false-negative rate was substantially lower. If the clipped node is not one of the sentinel lymph nodes, as is reported in approximately 25% of cases, then it is more likely that a false-negative result will be obtained with SLNB.
At first blush, the results of the ACOSOG Z1071 and SENTINA (Sentinel-Lymph-Node Biopsy in Patients With Breast Cancer Before and After Neoadjuvant Chemotherapy) trials[11,16] may seem to herald the end of SLNB after chemotherapy in patients with initially node-positive disease. However, before committing all of these patients to ALND after chemotherapy, one should consider an alternative approach. First, a clip should be placed in the index node at the time of diagnosis, and the number of abnormal nodes should be assessed; this is a surrogate for disease burden in that nodal basin. Second, response to chemotherapy should be assessed prior to surgical intervention, since those having obvious residual nodal disease are the most likely to benefit from ALND. Underlying tumor biology is also a factor, since patients with triple-negative disease and human epidermal growth factor receptor 2 (HER2)-positive breast cancer are more likely to experience pCR. Third, the clipped node should be targeted for removal at the time of SLNB, since a significant proportion of clipped nodes will not be sentinel lymph nodes. This may be due to fibrosis of lymphatic channels or to residual cancer burden blocking lymphatics.
The plan to target the clipped node for resection at the time of SLNB has been described as targeted axillary dissection by Caudle and colleagues.[18] This approach embraces the concept of individualized and multidisciplinary management of the breast cancer patient. The goal is to deliver the right treatment to all patients and spare them from unnecessary toxicities and long-term effects related to surgical management.
Financial Disclosure: Dr. Hunt serves on the Advisory Board for Armada Health.
References:
1. Swain SM, Sorace RA, Bagley CS, et al. Neoadjuvant chemotherapy in the combined modality approach of locally advanced nonmetastatic breast cancer. Cancer Res. 1987;47:3889-94.
2. Hunt KK, Ames FC, Singletary SE, et al. Locally advanced noninflammatory breast cancer. Surg Clin North Am. 1996;76:393-410.
3. Hennessy BT, Hortobagyi GN, Rouzier R, et al. Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J Clin Oncol. 2005;23:9304-11.
4. Kuerer HM, Sahin AA, Hunt KK, et al. Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann Surg. 1999;230:72-8.
5. Gianni L, Pienkowski T, Im YH, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13:25-32.
6. Manguso N, Gangi A, Giuliano AE. Neoadjuvant chemotherapy and surgical management of the axilla in breast cancer: a review of current data. Oncology (Williston Park). 2015;29:733-8;782.
7. Xing Y, Foy M, Cox DD, et al. Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg. 2006;93:539-46.
8. Kelly AM, Dwamena B, Cronin P, Carlos RC. Breast cancer sentinel node identification and classification after neoadjuvant chemotherapy-systematic review and meta analysis. Acad Radiol. 2009;16:551-63.
9. van Deurzen CH, Vriens BE, Tjan-Heijnen VC, et al. Accuracy of sentinel node biopsy after neoadjuvant chemotherapy in breast cancer patients: a systematic review. Eur J Cancer. 2009;45:3124-30.
10. Fu JF, Chen HL, Yang J, et al. Feasibility and accuracy of sentinel lymph node biopsy in clinically node-positive breast cancer after neoadjuvant chemotherapy: a meta-analysis. PLoS One. 2014;9:e105316.
11. Boughey JC, Suman VJ, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455-61.
12. Hunt KK, Yi M, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy is accurate and reduces the need for axillary dissection in breast cancer patients. Ann Surg. 2009;250:558-66.
13. Wolmark N, Wang J, Mamounas E, et al. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Nat Cancer Inst Monogr. 2001:96-102.
14. Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778-85.
15. van Nes JG, Putter H, Julien JP, et al. Preoperative chemotherapy is safe in early breast cancer, even after 10 years of follow-up; clinical and translational results from the EORTC trial 10902. Breast Cancer Res Treat. 2009;115:101-13.
16. Kuehn T. Bauerfeind I, Fehm T, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospectcive, multicentre cohort study. Lancet Oncol. 2013;14:609-18.
17. Boileau FJ, Poirier B, Basik M, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol. 2015;33:258-64.
18. Caudle AS, Yang WT, Mittendorf EA, et al. Selective surgical localization of axillary lymph nodes containing metastases in patients with breast cancer: a prospective feasibility trial. JAMA Surg. 2015;150:137-43.
Articles in this issue
over 10 years ago
Introducing the New-and-Improved ONCOLOGY Journalover 10 years ago
Javier Cortés, MD, on the CLEOPATRA Trialover 10 years ago
Bevacizumab and Glioblastoma: The Ecstasy and the Agonyover 10 years ago
Salivary Gland Cancers: The Challenges of Progress in Rare TumorsNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.