
FDA Grants Accelerated Approval to Pirtobrutinib for Relapsed/Refractory MCL
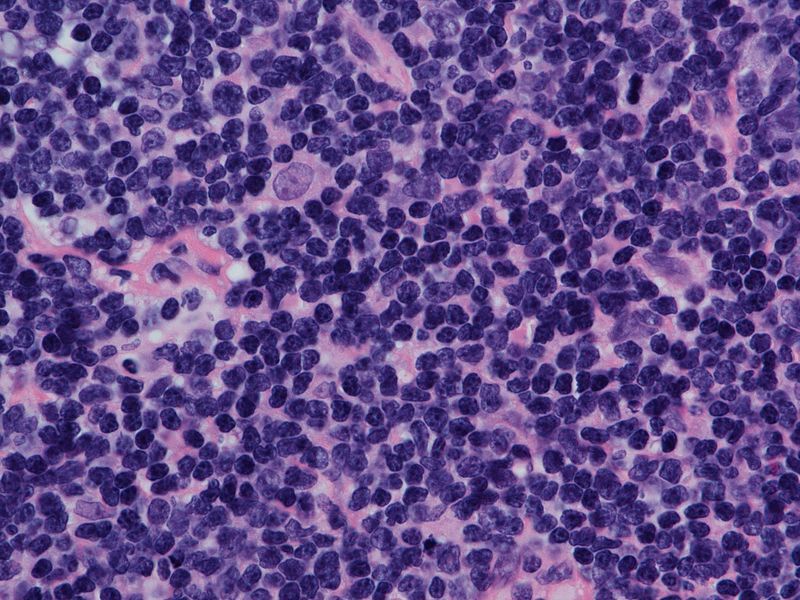
The approval for pirtobrutinib in the treatment of patients with relapsed or refractory mantle cell lymphoma was based on data from the phase 1/2 BRUIN trial.
The FDA has given accelerated approval to pirtobrutinib (Jaypirca) for the treatment of patients with relapsed/refractory mantle cell lymphoma (MCL) following at least 2 prior lines of therapy, according to a press release from the FDA.1
The approval for pirtobrutinib was supported by data from the phase 1/2 BRUIN trial (NCT03740529), in which investigators assessed the agent as monotherapy among patients previously treated with a Bruton tyrosine kinase (BTK) inhibitor.2 Investigators reported an objective response rate (ORR) of 50% (95% CI, 41%-59%), including a complete response rate of 13%. Additionally, the estimated median duration of response (DOR) was 8.3 months (95% CI, 5.7-not evaluable), and the 6-month DOR was 65.3% (95% CI, 49.8%-77.1%).
“The approval of [pirtobrutinib] represents an important advance for patients with relapsed or refractory MCL, who currently have limited options and historically have had a poor prognosis following discontinuation of treatment with a covalent BTK inhibitor,” Michael Wang, MD, Puddin Clarke Endowed professor of Lymphoma and Myeloma at the University of Texas MD Anderson Cancer Center, said.3 “These data indicate that Jaypirca can provide efficacy in patients previously treated with a covalent BTK inhibitor, potentially extending the time patients may benefit from BTK inhibition therapy.”
The FDA has approved a recommend dosage of 200 mg of oral pirtobrutinib once a day until progressive disease or unacceptable toxicity.
The primary end points of the BRUIN trial included the maximum tolerated dose, and recommended dose for further studies. Secondary end points include safety profile, pharmacokinetics, ORR, and DOR.
The most common adverse effects (AEs) observed in patients with MCL during the BRUIN trial included fatigue, musculoskeletal pain, diarrhea, edema, dyspnea, pneumonia, and bruising. Grade 3 or 4 AEs included decreased neutrophil counts, lymphocyte counts, and platelet counts.
“[Pirtobrutinib] offers a new approach to targeting the BTK pathway following treatment with a covalent BTK inhibitor and has the potential to meaningfully impact the treatment paradigm for relapsed and refractory MCL,” Wang concluded.
References
- FDA grants accelerated approval to pirtobrutinib for relapsed or refractory mantle cell lymphoma. News release. FDA. January 27, 2023. Accessed January 27, 2023. bit.ly/3Y4DVSw
- Loxo@Lilly presents updated pirtobrutinib data from the phase 1/2 BRUIN clinical trial at the 2022 American Society of Hematology Annual Meeting. News release. Lox@Lilly. December 12, 2022. Accessed January 27, 2023. https://bit.ly/3XH4Ow3
- U.S. FDA approves Jaypirca™ (pirtobrutinib), the first and only non-covalent (reversible) BTK inhibitor, for adult patients with relapsed or refractory mantle cell lymphoma after at least two lines of systemic therapy, including a BTK inhibitor. News release. Loxo@Lilly. January 27, 2023. Accessed January 27, 2023. bit.ly/3ReOGPC
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.





































