- ONCOLOGY Vol 15 No 4
- Volume 15
- Issue 4
Incidence of Pap Test Abnormalities Within 3 Years of a Normal Pap Test-United States, 1991-1998
Declines in cervical cancer incidence and mortality reported in the United States since the 1950s have been attributed to early detection and treatment of precancerous and cancerous lesions through the use of the Pap test. More than 50 million
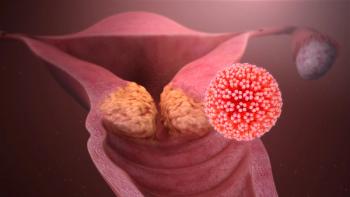
Declines in cervical cancer incidence and mortality reportedin the United States since the 1950s have been attributed to early detection andtreatment of precancerous and cancerous lesions through the use of the Pap test.More than 50 million Pap tests are performed each year; however, guidelinesabout the frequency of testing in women with a history of normal test resultsare inconsistent.
To determine the incidence of cervical cytologic abnormalitiesfollowing a normal Pap test, 1991 to 1998 data from the National Breast andCervical Cancer Early Detection Program (NBCCEDP) were analyzed for this report.The findings indicated that within 3 years of a normal Pap test result, severecytologic abnormalities were uncommon, and incidence rates were similar amongwomen screened 1, 2, and 3 years following a normal Pap test.
Demographics ofAnalysis Participants
For each woman, the Centers for Disease Control (CDC) received areport that included demographic characteristics, Pap test results, diagnosticprocedures, and histopathologic results. To be eligible for the analysis, womenwere required to have had a first NBCCEDP Pap test reported as normal between1991 and 1998, and at least one subsequent Pap test performed within thefollowing 9 to 36 months. Of 620,063 women tested between 1991 and 1998, 128,805(20.8%) met the criteria for eligibility. Results of Pap tests were reportedusing Bethesda System categories: normal; infection, inflammation, or reactivechanges; atypical squamous cells of undetermined significance (ASCUS); low-gradesquamous intraepithelial lesion (LSIL); high-grade squamous intraepitheliallesion (HSIL); "suggestive of squamous cell carcinoma"; and"other" (eg, glandular atypia and atypical endocervical glands).
Incidence rates of Pap test interpretations were calculated bydividing the number of women with each test result by the number of womenretested within each age group (< 30 years,30 to 49 years, 50 to 64 years, and ³ 65 years) and time interval (9 to12 months, 13 to 24 months, and 25 to 36 months). Incidence rates wereage-adjusted using the age distribution of the 1996 NBCCEDP population. Ordinaryleast-squared regression was used to evaluate the trend of increasing timebetween the first Pap test on the age-adjusted incidence of ASCUS, LSIL, HSIL,and suggestive of squamous cell carcinoma.
The average age of women included in the analysis was 48.9 years(range: 12 to 96 years); 73,631 (57.0%) were non-Hispanic whites; 22,672 (17.6%)were Hispanics; 17,314 (13.4%) were non-Hispanic blacks; 10,983 (8.5%) wereAmerican Indians/Alaska natives; 3,070 (2.4%) were Asians/Pacific Islanders, and1,135 (0.9%) were categorized as "other" or "unknown." Themean time between the first and second test was 15.7 months.
Results of Analysis
Approximately 121,576 (94.4%) of the 128,805 second test resultswere interpreted as normal or infection, inflammation, or reactive changes. Theincidence rate of the second test results interpreted as HSIL and suggestive ofsquamous cell carcinomas was 66 per 10,000 women aged < 30 years, 22 per10,000 women aged 30 to 49 years, 15 per 10,000 women aged 50 to 64, and 10per 10,000 women aged ³ 65 years (trend test, P < .001). Overall, as ageincreased, the incidence of ASCUS and LSIL also decreased (trend test, P <.001, each category).
The age-adjusted incidence of results interpreted as LSILincreased over time (trend test, P = .01) (Table1). The incidence of ASCUS, themost common cytologic abnormality, didnot change significantly over time (P = .36). The differences in the age-adjusted incidence of HSIL and suggestiveof squamous cell carcinoma for the time intervals were also not significant (P =.42).
Editorial Note From the CDC
The US Preventive Services Task Force recommends Pap testscreening at least every 3 years until age 65 years. The American Cancer Societyguidelines suggest that screening less frequent than annually may be adequatefor Pap testing in women with a history of three negative annual Pap tests, andthe American College of Obstetricians and Gynecologists recommends annual Paptests for most women.
The difference in screening annually, biennially, or trienniallyis substantial in the number of tests performed and in the public healthimplications. In this analysis, women screened 1, 2, and 3 years after a normalPap test had similar risk for developing HSIL and suggestive of squamous cellcarcinoma. Other studies have indicated clinically insignificant additionalprotection in testing yearly compared with triennially.
However, low-grade abnormal Pap results (eg, ASCUS and LSIL)constituted > 95% of the cytologic abnormalities after the first normalresults. The clinical significance of these abnormalities is unclear. Women whowere screened annually rather than less frequently might have worse healthoutcomes if low-grade results of undetermined clinical importance lead tofurther testing and unnecessary patient morbidity and anxiety.
Limitations of Findings
The findings in this report are subject to at least fourlimitations. First, the database used was intended for descriptive statisticsand not for hypothesis testing; data were limited to a few variables. Second,the NBCCEDP serves low-income and uninsured women; results may not begeneralizable to other groups. However, low-income and uninsured women usuallyare at greater risk of developing cervical neoplasia than women with higherincomes; therefore, higher-income women should be less likely to exhibit higherrates during the 3-year interval examined in this study.
Third, women may have received Pap testing outside the programduring the time between the first and subsequent Pap tests; however, thisprobably occurred in only a few women. Finally, women who frequently getscreened, specifically within 1 year after a Pap test, might be low-risk womenconcerned about their health or high-risk women with histories of abnormal Paptests who have been told to get annual tests.
Other risks for cervical cancer in these women and whether theserisks affected the findings in this study are unknown. The NBCCEDP receives datafrom many cytopathology laboratories and clinical settings. The findings in thisstudy may better represent actual clinical settings than the findings in acontrolled trial.
The CDC is working with state health departments to use thisinformation as a basis for cost-effective strategies to reach women who have notreceived screening services for cervical disease. The CDC will assist theNBCCEDP in assessing program-provider practices, modifying patient recallsystems, and developing professional and public education strategies to improvepatient-provider decision making. Further research is needed to clarify thebenefit and harm related to the frequency of subsequent Pap testing in womenwith normal results.
Articles in this issue
almost 25 years ago
Are Older Lymphoma and Breast Cancer Patients Undertreated?almost 25 years ago
SkyePharma and Chiron Announce Relaunch of Liposomal Cytarabinealmost 25 years ago
OvaRex Study Demonstrates Efficacy and Safety in Ovarian Cancer Patientsalmost 25 years ago
Health-Related Quality of Life in Cancer Clinical Trialsalmost 25 years ago
Managed-Care Reform...Againalmost 25 years ago
Chemotherapy Drugs Categorized as ‘In-Office Ancillary Services’almost 25 years ago
New Technology in Breast Cancer Testing Appears Promisingalmost 25 years ago
Thalidomide Studied in a Variety of Cancers and Metabolic DisordersNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.