Presentation: Tipifarnib in HNSCC With HRAS Mutations
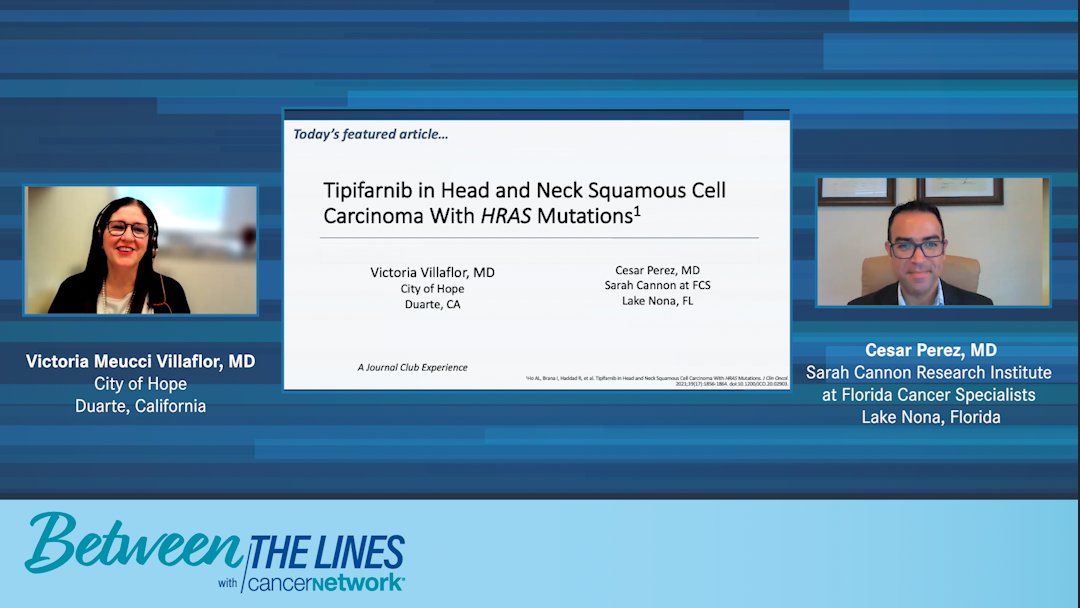
Drs Cesar Perez and Victoria Meucci Villaflor review “Tipifarnib in Head and Neck Squamous Cell Carcinoma With HRAS Mutations” by Ho AL, et al.
Victoria Meucci Villaflor, MD: Hello, and welcome to Between the Lines, a Journal Club Experience. Today’s featured article is, “Tipifarnib in Head and Neck Squamous Cell Carcinoma With HRAS Mutations.” My name is Dr Victoria Villaflor. I’m the section chief of head and neck oncology and professor in the Department of Medical Oncology and Therapeutics Research at City of Hope. I’m lucky to be joined by my colleague, Dr Cesar Perez. He‘s also a head and neck medical oncologist whom I’ve known for many years. He started out in Florida and has recently moved to the Sarah Cannon Research Institute at Florida Cancer Specialists, where he’s the director of drug development. Welcome, Cesar.
Cesar Perez, MD: Thank you so much, Vicky. It’s an honor to be here with you after all these years to discuss the result of this study that, although it’s small, is quite important in the field of head and neck medical oncology. It’s quite exciting.
Victoria Meucci Villaflor, MD: Dr Perez, do you want to give us some background about this drug before we get into the study?
Cesar Perez, MD: Yes. Tipifarnib is what’s called a signal transduction inhibitor, specifically a farnesyltransferase inhibitor. If you don’t know, you might think it inhibits HRAS directly, but this drug was developed 20 years ago. There were large trials that included patients with RAS mutations, both KRAS and NRAS, which unfortunately weren’t found to be effective. There was no efficacy of the farnesyltransferase inhibitor. It’s slightly explained because the preclinical data demonstrated that NRAS and KRAS are susceptible for alternative farnesylation events.
But the HRAS mutation is uniquely dependent on farnesylation alone. All HRAS mutations aren’t the same, and the HRAS abnormality in patients with head and neck squamous cell carcinoma depends on this specific enzyme being active. That’s what tipifarnib does, which is interesting because it’s at least 2 decades old, and it took all this time for us to find this specific target. It’s a very interesting drug and an interesting finding to be discussed.
Victoria Meucci Villaflor, MD: It’s an interesting drug. For people who treat a lot of lung cancer, the struggles we’ve had over the years with all of the RAS mutations—as Dr Perez had pointed out, the KRAS, NRAS, and HRAS—getting direct targeting of any of these particular RAS-signaling genes has been rather difficult. The FDA breakthrough designation for sotorasib and KRAS was really interesting. Unfortunately, only less than 2% of all head and neck squamous cell carcinomas have any kind of KRAS mutation, so it’s been a difficult process there. And only between 4% and 8% have HRAS. So this has been a very interesting trial.
As far as the study, it was recently published by another friend and colleague, Alan Ho, [MD, PhD,] out of Memorial Sloan Kettering Cancer Center. What was initially done was a study looking at patients with HRAS-mutated tumors, and they were solid cancer tumors. The first cohort was thyroid cancer, the second cohort was all solid tumors other than thyroid cancer, and the third cohort was squamous cell cancer other than head and neck squamous cell carcinoma. During the development of the study, there were a number of patients with head and neck squamous cell carcinoma enrolled. What initially was found was in the total of the first 9 patients enrolled at interim analysis, 5 of those patients with head and neck squamous cell carcinoma and HRAS mutations had a response to tipifarnib. This cohort was then expanded, and the total number of patients who were involved in this cohort was 31.
During the development of these 31 patients, there were also some other data that were analyzed at the initial analysis. What was notable about those first 5 of 9 patients who were responding is they had a variable allele frequency of HRAS mutations of greater than or equal to 20%. Hence during this cohort expansion, there were an additional 22 patients who were put on this study with a variable allele frequency of greater than or equal to 20%. Once the patients were evaluated for efficacy, there were 20 patients analyzed; of those 20 patients, 11 had a partial response and 9 had stability of disease, which is really impressive.
Of the 9 patients enrolled with a variable allele frequency of less than or equal to 20%, there were 4 who were evaluable for efficacy. And of those patients with low variable allele frequency, 2 had stable disease and 2 had progressive disease. Five were not evaluable for efficacy in that group. The demographics of the patients who had high variable allele frequency head and neck squamous cell carcinoma were that 68% of the patients were male, the median age was 63, the age range was 20 to 89, and 90% of the patients were evaluable for efficacy.
As far as the site of the primary tumor, 45.5% were oral cavity, 18.2% were pharynx, 13.6% larynx, and 22.7% were other. The number of prior anticancer treatments ranged anywhere from 0 to 6, with a median of 2. The type of prior anticancer therapies included platinum-based therapy in almost 91% of the patients, immunotherapy in approximately 64%, and cetuximab in 50%. HPV [human papillomavirus] status was available in 62% of the patients. And of those 13 patients who had available HPV status, 30.7% were positive and 69.2% were negative.
These plots and efficacy outcomes show that many of the tumors actually change in size. And what’s also noticeable about these is that the variable allele frequencies are higher in patients who generally have a response. Also noticeable is most of the patients are having a response, which is unusual in this population. The duration of response to treatment showed some correlation with variable allele frequency, but it’s not 100%, because all those variable allele frequencies have varying percentages and it doesn’t necessarily correlate with how long the duration of response to treatment is. Nonetheless, patients who have the higher variable allele frequencies do have a better duration of response to treatment, as long as it’s over 20%. I don’t know if you have anything to add to that, Cesar.
Cesar Perez, MD: Yes. Despite the small size of the study, this waterfall plot is what makes the study so compelling. This is what we want in every trial in oncology. On the left, we can see that 3 patients have no shrinkage, but their increase in size was stable disease paresis. All the other patients actually had a tumor shrinkage. Interestingly, when you see the patients with a little diamond, those were the ones treated with 600 mg. Initially, the study started with 900 mg and then switched to 600 mg because of tolerance. We can see there that many of the patients who have partial responses were actually treated with the 600-mg dose. It was obviously a good decision based on the outcomes of the study. It’s very promising. It’s the part that’s very exciting about this study.
Victoria Meucci Villaflor, MD: The efficacy outcomes, progression-free survival is also interesting. In a very small study, we have a progression-free survival with tipifarnib of 5.6 months in patients who are pretty heavily pretreated. Additionally, in patients on their last prior therapy, the progression-free survival is 3.6 months, which gives you an indication of how these patients generally behave. These are very compelling data in a very small number of patients. Do you have anything to add to that, Dr Perez?
Cesar Perez, MD: Yes. Initially, we don’t like to be adding data to patients on a Kaplan-Meier curve that weren’t collected directly from the trial. But these data of the last prior therapy are very important because, as you mentioned, these are patients who were pretreated before and were progressing fairly rapidly. That at least shows us that they had close to a 6-month progression-free survival, which is very important and significant.
Victoria Meucci Villaflor, MD: As far as the primary outcome response rate, the objective response rate was 55% in tipifarnib in patients who had a high variable allele frequency. The median progression-free survival was 5.6 months as depicted by the earlier progression-free survival curve with a 95% confidence interval of 3.6 to 16.4. As Dr Perez pointed out, these patients are pretty heavily pretreated in many instances. Progression-free survival on the last prior chemotherapy was 3.6 months with a 95% confidence interval of 1.3 to 5.2. Overall survival was 15.4 months in this group of patients, with a 95% confidence interval of 15.4 to 29.7.
As far as the adverse effects in 30 patients, as Dr Perez pointed out, they’re on 2 different doses of medications. Some had a higher dose than what ended up being the dose that’s going to be developed with this drug. Overall, the adverse effects have been cell count decreases, specifically anemia and neutropenia; different metabolic or nutrition disorders, such as hypercalcemia, hypokalemia, hypophosphatemia; and 3 patients developed pneumonia and GI [gastrointestinal] upset in the form of nausea. None of these were grade 3 or 4 as I recall, right?
Cesar Perez, MD: Yes, most of them actually got better with the lower doses. We talked about cytopenias. These are heavily pretreated patients, so it’s common for them to have cytopenias at this point with whatever treatment you give them. There doesn’t seem to be much severe toxicity with the drug, which is obviously a good thing in this population.
Victoria Meucci Villaflor, MD: What types of conclusions could we come up with from this paper?
Cesar Perez, MD: Again, it’s a small study, but the findings are quite compelling. It’s very interesting. It’s a target that was thought of as not able to be drugged. Now we can actually inhibit with this drug that is 20 years old. One of the main important issues from this study is that the practicality of next-generation sequencing for patients with head and neck squamous cell carcinoma had been put in doubt. How much can you use it? How much value do we get? With these findings, this is now an important tool for this population, because it seems that we finally have a targeted mutation that we can actually use in patients with head and neck squamous cell carcinoma.
Victoria Meucci Villaflor, MD: This small trial has been very intriguing. In all the years that I’ve been treating head and neck cancer and doing molecular studies, what I’ve found is there’s a very small group of patients in my practice, probably about 5% or 6% of patients—the reported numbers are between 4% and 8%—who have these HRAS mutations. Most of them do very poorly. One case that comes to my mind was a very young girl who had 3 young kids at home who had one of these HRAS mutations. No matter what I did for her, she just grew through it, and unfortunately succumbed to this awful disease. The fact that we have some data in a small study showing that we might be able to target this gene is very compelling. I look forward to further studies in this area as well to see if we can ultimately get this drug approved in this indication.
Cesar Perez, MD: Definitely. Most of the head and neck oncology field and specialists are waiting for more data about this. Hopefully it’ll translate into the clinic.
Transcript edited for clarity.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.
Related Content


Comparing Quality-of-Life Outcomes With Protons vs Photons in OPSCC

Subcutaneous Amivantamab Earns Breakthrough Therapy Designation in HNSCC