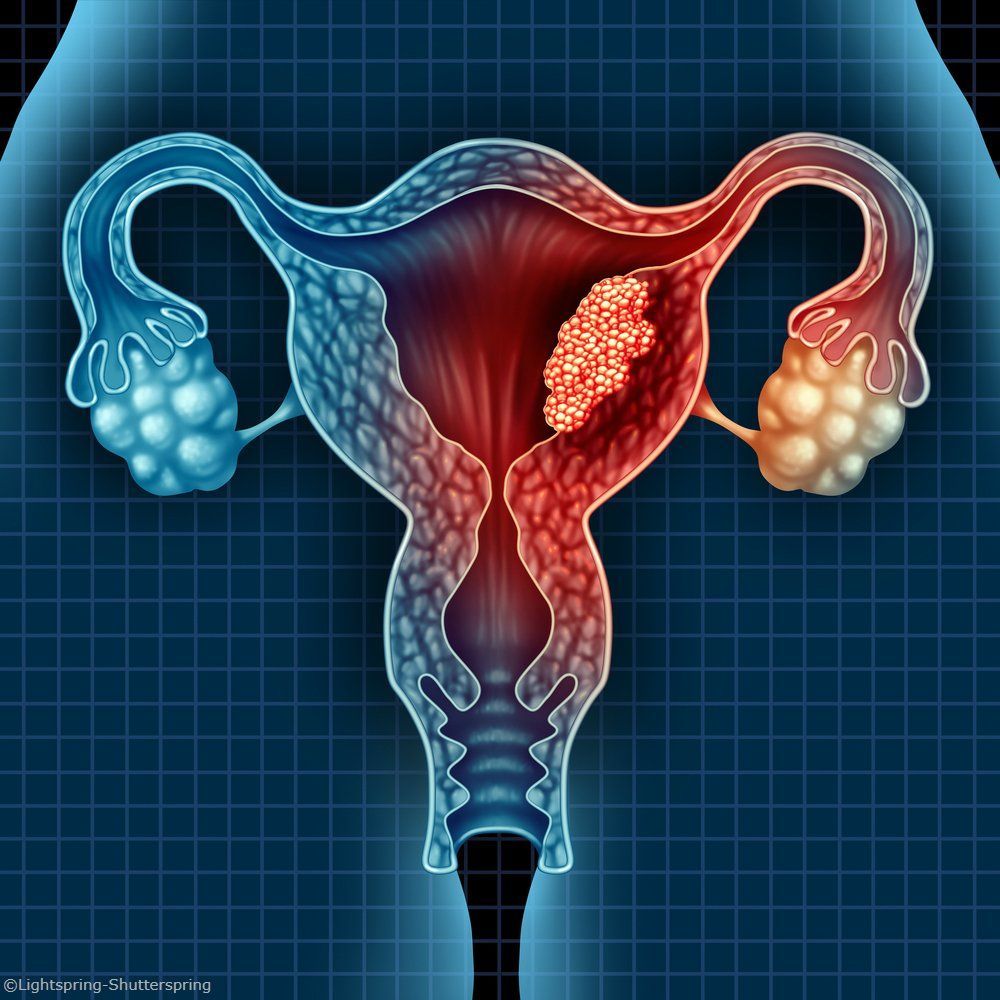
Retrospective Data Show Real-World Disparities in Black vs White Patients With Endometrioid Endometrial Carcinoma
SEER data showed that Black patients endometrioid endometrial carcinoma had higher 5-year cancer-related death rates compared with their White counterparts.
Endometrioid endometrial carcinoma
Black patients with endometrioid endometrial carcinoma in both real-world registries and GOG/NRG randomized phase 3 studies were found to have a significantly higher risk of death compared with White patients, despite propensity score matching. The retrospective findings were presented during the 2024 SGO Annual Meeting on Women’s Cancer.
Data from the Surveillance, Epidemiology, and End Results Program (SEER) revealed that Black patients (n = 4397) experienced a 5-year cancer-related death rate of 14.4% compared with 7.2% among White patients (n =47,959; HR, 2.04; 95% CI, 1.87-2.23; P < .0001). Moreover, the non-cancer death rate was also higher for Black patients compared with White patients, at 6.3% vs 4.6%, respectively (HR, 1.22; 95% CI, 1.09-1.36; P = .0007).
Additionally, Black patients in the National Cancer Database (NCDB; n = 13,468) experienced a worse overall survival (OS) probability compared with White patients (n = 155,706) in the original cohort before propensity score matching (HR, 1.52; 95% CI, 1.46-1.58). After propensity score matching, White patients (n = 13,468) still experienced a longer OS probability compared with Black patients (n = 13,468; adjusted HR, 1.29; 95% CI, 1.23-1.36).
“Endometrial cancer is one of the most common cancers among women in the United States with both rising incidence and mortality,” lead study author Zachary A. Kopelman, DO, FACOG, a gynecologic oncology fellow at Walter Reed National Military Medical Center in Bethesda, Maryland, wrote in the presentation. “Endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy in the US in 2024. Black patients with endometrial cancer are significantly more likely to have: aggressive histologic subtypes, high-grade tumors, and advanced stage disease.”
Black and White patients in real-world registries with endometrioid endometrial carcinoma who underwent hysterectomy with or without adjuvant treatment were eligible for the study. This trial included cohorts of patients from SEER from 2004 to 2016, NCDB from 2004 to 2017, NCI-sponsored phase 3 clinical trials, and from the Genomics Evidence Neoplasia Information Exchange (GENIE) project v13.0.
To conduct their study, investigators used standard statistical methods to compare variables and outcomes of interest across the 4 cohorts. In the NCDB cohort, propensity-score matching was performed according to age, comorbidity score, neighborhood income, insurance status, year of diagnosis, tumor grade, stage, lymphovascular space invasion, lymphadenectomy, and adjuvant treatment. Patients enrolled in randomized clinical trials were exactly matched by grade, stage, and treatment, and balancing was performed according to diagnosis and performance status. Study authors also adjusted matching for confounding effects caused by covariates.
Kopelman stated that the study’s objectives were to investigate disparities in cancer-related deaths, non-cancer deaths, survival, and molecular features in Black and White patients with endometrioid endometrial carcinoma in real-world registries, as well as to evaluate disparities in progression-free survival (PFS) and OS in Black and White patients with endometrioid endometrial carcinoma in NCI-sponsored randomized clinical trials.
Additional findings from the study showed that Black patients had a disproportionately lower enrollment in randomized clinical trials compared with White patients. There were less Black patients than White patients across the GOG-LAP2 (58 vs 1534, respectively), GOG-0249 (39 vs 313), GOG-0122 (20 vs 160), GOG-0184 (10 vs 353), GOG-0107 (15 vs 107), GOG-0139 (16 vs 133), GOG-0163 (13 vs 131), and GOG-0177 (16 vs 146) study protocols.
Across the randomized clinical trials, Black patients experienced a worse PFS compared with White patients in both the original cohort (HR, 2.05; 95% CI, 1.67-2.52) and the matched cohort (adjusted HR, 1.22; 95% CI, 0.99 -1.50). Additionally, Black patients in the original (HR, 2.19; 95% CI, 1.77-2.71) and matched cohort (adjusted HR, 1.32; 95% CI, 1.09 -1.61) experienced a shorter OS compared with White patients.
Results from the GENIE project demonstrated that Black patients had a significantly lower rate of PTEN (P = .029), PIK3R1 (P = .043), FBXW7 (P = .029), NF1 (P = .007), mTOR (P = .043), CCND1 (P = .029), and PI3K pathway related gene mutations compared with White patients. Mutations in TP53 (P = .371), DNA-repair-related genes (P = .841), and proportions of tumor mutational burden-high patients (P = .371) were similar between Black and White patients. Kopelman wrote that although multiple mutations were less frequent in Black patients, mutations still occurred at high frequency in these patients and that immune checkpoint inhibitors should be equally considered in this population.
Kopelman noted that the study was limited by the evaluation of single histologic subtype, range in years of diagnosis for the cohorts, exclusion of non–surgically managed patients, and exclusion of other race groups and ethnicities. Additionally, the study did not include more recently completed randomized clinical trials investigating agents such as immune checkpoint inhibitors or antibody-drug conjugates.
“Our investigation highlights racial disparities in clinical characteristics, molecular alterations, and survival outcomes between Black and White women with endometrioid endometrial carcinoma,” Kopelman wrote in his conclusion. “These disparities merit additional research on molecular features, exposures, lifestyle, biology, and societal factors. Drug development strategies targeting the common mutations and pathways in endometrioid endometrial carcinoma are needed with approaches to modify social determinants and enhance diverse inclusion in randomized clinical trials.”
Reference
Kopelman ZA. Disease progression, survival, and molecular disparities in black and white patients with endometrioid endometrial carcinoma in real-world registries and GOG/NRG Oncology randomized phase III clinical trials. Presented at: 2024 SGO Annual Meeting on Women’s Cancer; March 16-18, 2024; San Diego, CA.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.