
Results of prospective, open-label trial of olaparib maintenance in patients with platinum-sensitive relapsed ovarian cancer continued to demonstrate efficacy of the PARP inhibitor in this setting.

Your AI-Trained Oncology Knowledge Connection!


Results of prospective, open-label trial of olaparib maintenance in patients with platinum-sensitive relapsed ovarian cancer continued to demonstrate efficacy of the PARP inhibitor in this setting.

CancerNetwork® sat down with Jeffrey Graham, MD, FRCPC, to discuss the effectiveness of immune checkpoint inhibitors as frontline therapy for non–clear cell renal cell carcinoma
CancerNetwork® discussed updates in the treatment of gynecologic cancers with Ursula A. Matulonis, MD.

Novartis announced that its investigational targeted radioligand therapy 177Lu-PSMA-617 demonstrated statistically significant improvements in overall and radiographic progression-free survival versus standard-of-care therapy in patients with progressive PSMA-positive metastatic castration-resistant prostate cancer.
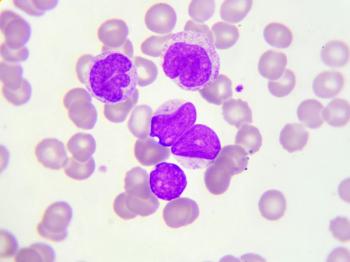
Children, adolescents, and young adult patients in first B-cell acute lymphoblastic leukemia relapse did not experience a statistically significant disease-free survival benefit with blinatumomab treatment compared with chemotherapy.

Adjuvant immunotherapy treatment was associated with a significant survival benefit for patients with stage II melanoma in a study presented at the Society of Surgical Oncology 2021 International Conference on Surgical Cancer Care.

Based on positive overall and progression-free survival data from the phase 3 KEYNOTE-590 trial, pembrolizumab was approved by the FDA for use in patients with metastatic or locally advanced esophageal or gastroesophageal junction carcinoma.
In a phase 1 trial, the recommended phase 2 dose of glofitamab resulted in frequent and durable complete responses for patients with follicular lymphoma and transformed diffuse large B-cell lymphoma arising from follicular lymphoma.

Take a look back at some of the important news and notes from last week in the world of oncology, featuring news about breast cancer, prostate cancer, molecular profiling, ovarian cancer, and more.

The combination of cediranib and olaparib demonstrated modest efficacy in patients with recurrent, metastatic, or persistent endometrial cancer; however, this was not significantly different compared to cediranib alone.

Results of the phase 3 IMpower010 trial have demonstrated that adjuvant atezolizumab for patients with stage IB to IIIA non–small cell lung cancer leads to increased disease-free survival versus best supportive care for patients with high PD-L1.
PFS improvement as well as a trend to overall survival prolongation has been demonstrated with niraparib maintenance in patients with platinum-sensitive recurrent ovarian cancer with or without germline BRCA mutations.

Although responses were limited in patients with paclitaxel-pretreated cervical cancer, eribulin may still show promise in those who are naïve to treatment with the chemotherapy agent.

Data from the phase 2 OVARIO study showed extended progression-free survival benefit of niraparib plus bevacizumab in patients with heavily pretreated advanced ovarian cancer.

A dostarlimab triplet combination showed promise in a phase 2 study for treatment of patients with platinum-resistant ovarian cancer, according to a presentation at the Society of Gynecologic Oncology 2021 Virtual Annual Meeting on Women’s Cancer.
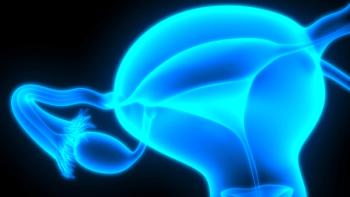
An update from the phase 3 ARIEL4 trial presented at the Society of Gynecologic Oncology 2021 Virtual Annual Meeting on Women’s Cancer supports the continued use of rucaparib in patients with BRCA-mutant relapsed advanced ovarian cancer, based on progression-free survival and response data.

Patients with newly diagnosed ovarian cancer who had interval debulking surgery and visible residual disease showed promising outcomes when treated with the PARP inhibitor niraparib, according to a post hoc analysis of a phase 3 clinical trial.

Compugen announced updated data surrounding the investigational therapeutic antibody, COM701, as monotherapy and in combination with nivolumab.

Following a prior announcement that the phase 3 KEYNOTE-775 trial met both primary end points of progression-free and overall survival benefit, data for the pembrolizumab/lenvatinib combination were presented at the Society of Gynecologic Oncology 2021 Annual Meeting on Women’s Cancer.

Data presented at the Society of Surgical Oncology 2021 International Conference on Surgical Cancer Care found that breast pCR was predictive of nodal pCR for patients with HER2-positive and triple-negative breast cancer treated with chemotherapy.

CancerNetwork® sat down with Thomas Hutson, DO, PharmD, to discuss results of the CLEAR trial presented at the recent Genitourinary Cancers Symposium.
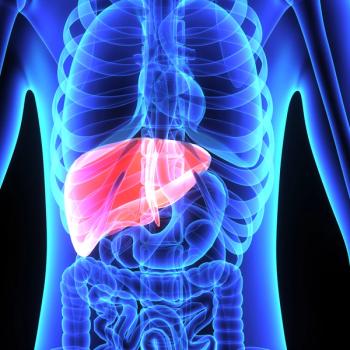
Based on a single-institution study, investigators were able to correlate outcomes for unresectable colorectal liver metastases with the addition of hepatic arterial infusion pump therapy to systemic therapy to the presence of a mutation in KRAS.

One year after surgery, patients aged 70 years or older experienced moderate-to-severe tiredness, poor well-being, and lack of appetite.

A selective internal radiation therapy from Boston Scientific Corporation, TheraSphere Y-90 Glass Microspheres, was granted FDA approval for the treatment of unresectable hepatocellular carcinoma.

Exelixis recently announced that cabozantinib received a breakthrough therapy designation from the FDA based on data from the COSMIC-311 trial for the treatment of differentiated thyroid cancer.

A novel imaging technology was cleared by the FDA to detect polyps with neoplastic potential during conduct of colonoscopy that aligns with pathological assessment with greater than 90% predictive ability.

Recently reported results from the ongoing phase 1 TUNINTIL trial of the oncolytic virus TILT-123 show safety of this approach.
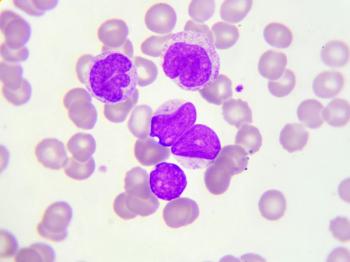
“As the first AML trial to use MRD negative CR as a primary endpoint, our trial is breaking new ground that may help deliver effective, targeted therapies more expeditiously to patients living with this devastating disease,” Bischofberger said.

CancerNetwork® sat down with Conor E. Steuer, MD, to discuss a recently published prospective study which found a high rate of smoking reduction and cessation in patients with non–small cell lung cancer.

The FDA accepted a new drug application for belzutifan to treat von Hippel-Lindau disease¬–associated renal cell carcinoma and granted it priority review based on response rate results from a phase 2 trial.