Oncology NEWS International
- Oncology NEWS International Vol 16 No 9
- Volume 16
- Issue 9
WT1 peptide vaccine produces durable disease control in some patients with AML or MDS; a phase II study is on the horizon
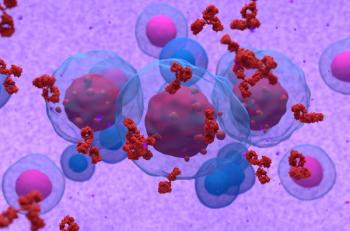
An HLA-A2-restricted peptide vaccine given as salvage therapy to patients with acute myeloid leukemia or myelodysplastic syndrome showed evidence of immunological, molecular, and clinical efficacy
ASCOAn HLA-A2-restricted peptide vaccine given as salvage therapy to patients with acute myeloid leukemia or myelodysplastic syndrome showed evidence of immunological, molecular, and clinical efficacy, German investigators reported at ASCO 2007 (abstract 3008).
By week 10 after starting a series of vaccinations, more than half the patients experienced an immunological response, and, for many, these were accompanied by a relapse-free period lasting several months, reported Ann Letsch, MD, of Charite Campus Benjamin Franklin, Universitatsmedizin, Berlin.
The HLA-A2-restricted WT1.126-134 peptide may represent "close to an ideal tumor antigen," Dr. Letsch said. WT1 is an embryonic transcription factor that is highly expressed in AML (driving blast proliferation) and various carcinomas. WT1-specific T cells lyse only AML blasts and not stem cells, and the vaccine has not shown toxicity in animal models.
Her study included 29 patients with WT1-expressing AML or MDS with an IPS score ≥ 1.5 or WTI expression in the peripheral blood. Patients were not candidates for stem cell transplant and had no other reasonable treatment options. All were HLA-A2 positive.
The patients received the WT1 peptide 0.2 mg on day 3, plus GM-CSF 75 µg/d on days 1-4 as a dendritic cell stimulant, and 1 mg KLH on day 3 as a T-helper protein.
The first cohort (n = 13) received the vaccine every 2 weeks for 4 weeks, then every 4 weeks thereafter. The second cohort received the vaccine every 2 weeks for 12 weeks, and every 4 weeks thereafter (n = 16). Patients experiencing disease progression could continue to receive up to six vaccinations if inclusion criteria were still met and chemotherapy was not required.
The cohorts were combined in the final analysis at week 10, which included 26 patients for efficacy, 23 for mRNA WT1 levels, and 25 for T-cell response.
"We chose to measure this at an early time pointafter four to five vaccinationsto guarantee having a comparison that included all the patients," she said.
A WT1-tetramer response of twofold or higher of the prevaccine response was observed in 52% of the whole study population. This percentage rose to 72% in the subset of patients who lacked a preexisting WT1-specific response prior to vaccination. Patients without a preexisting WT1-specific response also demonstrated cytokine production post-vaccination. The vaccine did not boost the WT1 T-cell response in any of the patients with a preexisting response.
The molecular response paralleled the clinical course, Dr. Letsch said, with a number of patients achieving durable disease control. Among the responders, a 10-fold or greater reduction in WT1 levels was seen in 33% of patients. One 67-year-old woman with AML who was in her second partial remission post-chemotherapy had a clear T-cell response and disease stabilization lasting 17 months.
Among 18 patients with active disease, 13 showed evidence of response to the vaccination, with 1 patient achieving complete remission and 12 having stable disease lasting at least 2 months. Among this group of 18 patients, 8 with untreated or secondary AML had disease stabilization lasting up to 7 months and 4 of them had a 50% or greater reduction in blasts.
Two patients with MDS mounted a major response, and one had a 50% reduction in blasts in the peripheral blood.
In the 8 AML patients, who had a complete remission after chemotherapy but were at high risk of relapse, time to treatment failure after vaccination ranged from 2 months to 10+ months. "In one very impressive case, disease stabilization has continued for over 38 months," Dr. Letsch noted. Further, she said, "the greater the reduction in WT1 level, the longer the time to treatment failure."
The investigators are initiating a randomized phase II study in high-risk AML patients in first or second remission, comparing HLA-A2-positive patients receiving the vaccine with HLA-A2-negative controls.
Articles in this issue
over 18 years ago
Low circulating levels of IGFBP-1 predict risk of pancreatic cancerover 18 years ago
Loss of two hormones creates a 'recipe for colon cancer'over 18 years ago
Monitoring essential for heading off retinoic acid syndromeover 18 years ago
Website helps you evaluate EMR systems for possible purchaseover 18 years ago
MRI accurately detects high-grade DCISover 18 years ago
Phase II trial to evaluate four-drug therapy in myelomaover 18 years ago
Novel optical technology detects treatable pancreatic caover 18 years ago
Xeloda/Avastin moderately active in advanced breast cancerover 18 years ago
Neuvenge active in refractory HER2+ breast caNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.