
A reduced estimated glomerular filtration rate (eGFR) was found to be associated with a significantly increased risk for renal and urothelial cancer, according to the results of a recently published study.

Your AI-Trained Oncology Knowledge Connection!


A reduced estimated glomerular filtration rate (eGFR) was found to be associated with a significantly increased risk for renal and urothelial cancer, according to the results of a recently published study.

An increased intake of vitamin A may result in a decreased risk for bladder cancer, according to the results of a meta-analysis.
Neoadjuvant treatment with dose-dense methotrexate, vinblastine, doxorubicin, and cisplatin was well tolerated and should be considered a reasonable option for patients with muscle-invasive urothelial cancer, according to a new study.

A noninvasive DNA methylation test using urine samples from patients with non–muscle-invasive bladder cancer can detect cancer recurrence. The test demonstrated both specificity and sensitivity in detecting recurrence.
In an early trial, a patient with bladder cancer has had a 14-month complete response to treatment with the mTOR inhibitor everolimus.
A new study found that induction bladder-conserving treatment was safe in patients with muscle-invasive bladder cancer who achieved only a near-complete response.
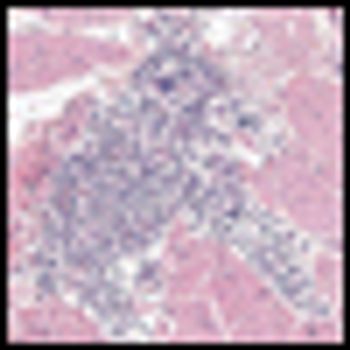
As part of The Cancer Genome Atlas project, a new study aimed at understanding the molecular basis of bladder cancer has identified several potential drug targets.
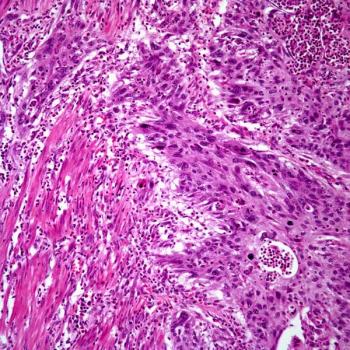
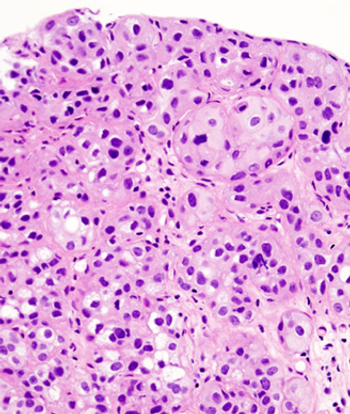
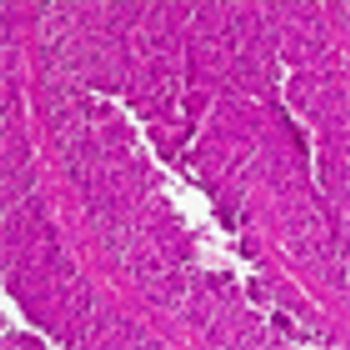
A 76-year-old woman with a history of dementia, hypertension, type 2 diabetes mellitus, and newly diagnosed squamous cell carcinoma of the urinary bladder was referred to Indiana University Medical Center after 3 to 4 weeks of hospitalization at two other hospitals.
A 55-year-old woman with a history of metastatic melanoma in remission for 8 years presented to the emergency department with gross hematuria. A CT scan, ordered because the patient was in menopause, demonstrated a bladder tumor.

There will always be patients who are either not surgical candidates or who refuse radical cystectomy, but in all other cases radical extirpative surgery should be the preferred management for patients with HGT1 disease who fail to respond to intravesical bacillus Calmette-Guérin therapy.

Decades of experience now exist to support the use of chemoradiotherapy in the treatment of muscle-invasive bladder cancer. Chemoradiotherapy for T1 tumors that recur following bacillus Calmette-Guérin therapy is promising and provides an important curative alternative for those unable or unwilling to undergo radical cystectomy.

General practitioners took longer to suspect a diagnosis of bladder or renal cancer in women compared with men, according to a recent study.
Recent studies suggest patients with bladder cancer are not receiving optimal care or the follow-up surveillance as recommended by the National Comprehensive Cancer Network (NCCN).

The use of cannabis among men has been linked to a significantly decreased risk for bladder cancer, according to a recent study; however, no cause and effect association has been found.

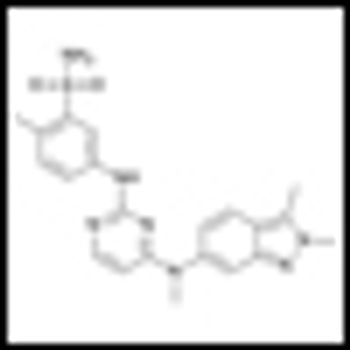
This review focuses on targeted therapies related to these pathways of interest for the treatment of advanced urothelial carcinoma, describing the evidence to support further investigation of these approaches.

Current efforts utilizing genomic strategies to unravel the biology of urothelial carcinoma will undoubtedly lead to rational targets, new therapies, and a renewed enthusiasm among researchers and clinicians working in this field-which ultimately will improve the lives of patients with this devastating disease.

Advanced urothelial cancer remains, along with pancreatic cancer, one of the last solid tumors for which essentially no progress has been made for 25 years. It’s time to think out of the box, and to develop novel and creative ways of overcoming the real, but not insurmountable, logistical challenges to carrying out the needed clinical trials.

In a trial of 64 patients, neoadjuvant chemotherapy with methotrexate, doxorubicin, vinblastine, and cisplatin (MVAC) had promising results in the treatment of muscle-invasive bladder cancer.

The use of presurgical characteristics to assign the clinical stage of a patient with bladder cancer was found to be highly inaccurate with a clinical/pathological stage discrepancy rate of 47.8% found in a large sample of patients taken from the National Cancer Data Base between 1998 and 2009.
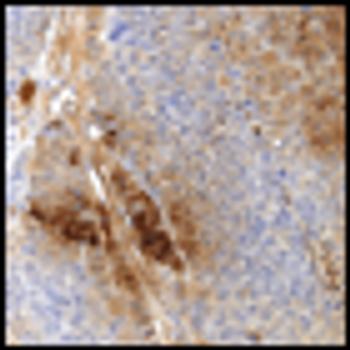
Researchers have identified bladder cancer markers that can predict which patients may have the most aggressive, fatal type of the disease. It was also discovered that smoking can affect the course of bladder cancer development, leading to more aggressive forms of the disease.

In a multicenter phase III trial of 360 patients with muscle-invasive bladder cancer, synchronous chemoradiotherapy provided better locoregional control without significant added toxicity, investigators for the Bladder Cancer 2001 trial have found.
The antiangiogenic agent pazopanib demonstrated clinically meaningful activity in patients with refractory urothelial cancer in a phase II proof-of-concept study, identifying pazopanib as the first targeted compound to have clinically meaningful activity in patients with refractory urothelial cancer.

Muscle-invasive bladder cancer is an aggressive and potentially lethal disease. Integration of multimodal therapies, improved surgical techniques, and utilization of targeted agents has tremendously improved outcomes.

Patient selection based on a much more comprehensive biologic assessment of both host and tumor is likely the key to further advances in the treatment of all bladder cancer patients. Until such time, there can be no compromise in the careful application of the rigorous therapy required to optimize outcomes.

Still missing in our treatment of bladder cancer are the tools to accurately predict response to a specific therapy, whether it be chemotherapy, radiation, or transurethral resection alone. Once we have these tools, we will be well on our way to applying a more intelligent, true personalized medicine approach to the treatment of this disease.