
Participating in a palliative care consultation significantly decreased healthcare use of Medicare beneficiaries with advanced cancer at the end of life.

Your AI-Trained Oncology Knowledge Connection!


Participating in a palliative care consultation significantly decreased healthcare use of Medicare beneficiaries with advanced cancer at the end of life.

In both primary care and oncology settings, screening patients for sleep-wake disturbances comorbid with cancer and their daytime consequences can reduce the economic burden of untreated sleep problems.

A meta-analysis has found that exercise and psychological interventions were best at reducing cancer-related fatigue and were more effective than pharmaceutical options.

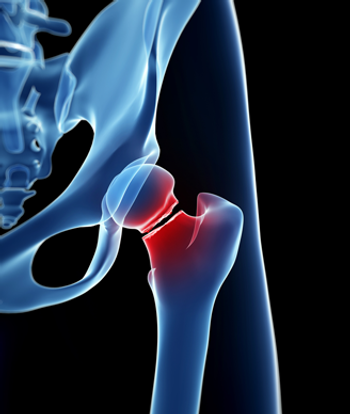
Men with painful bone metastases from prostate cancer may be able to achieve clinically meaningful improvements in pain and quality of life as early as 10 days after undergoing radiotherapy.

In this interview we discuss the different types of T-cell lymphomas and how supportive care is used in the management of these malignancies.

Acupressure, a technique derived from acupuncture, helped improve sleep and relieved chronic fatigue experienced by women treated for breast cancer.

The diagnosis and treatment of depression in the cancer setting can improve patients’ quality of life, their adherence to therapy recommendations, and the illness experience, all of which may affect survival outcomes.
In this video we discuss how palliative care early on in the process of treating patients with cancer led to an improvement in depressive symptoms and quality of life among family caregivers.

Early palliative care in cancer patients led to an improvement in depressive symptoms and quality of life among family caregivers.

The FDA has approved the first single-dose intravenous NK1 receptor antagonist, fosaprepitant dimeglumine (Emend), for the treatment of nausea and vomiting that can accompany the use of moderately and highly emetogenic chemotherapy.

In this interview we discuss the use of video to facilitate shared decision-making in the palliative care setting and improve patient understanding regarding goals of care.

A drug commonly given to cancer patients to relieve opioid-induced constipation is capable of slowing tumor growth and may play a role in developing new drug therapies.

Palliative care should be provided with cancer care early in the course of illness for all patients with advanced disease, according to a new guidance statement from ASCO and the American Academy of Hospice and Palliative Medicine.

A novel program combining radiation oncology with palliative care in patients with painful bone metastases increased the use of proven treatments while maintaining pain management, decreased palliative radiation use, and decreased hospital length of stay.

Almost 40% of patients undergoing palliative radiotherapy to treat symptomatic bone metastases experienced pain flare, according to an observational study.

According to a recent study, treatments aimed at preventing skeletal-related events in patients with advanced cancer and bone metastases could reduce pain and the need for opioids.
Results of a single-institution study found the risk for fracture among survivors of hematopoietic stem-cell transplantation increased by nearly eight times.

The best management of distress in a lung cancer patient involves aggressive physical symptom control, attention to concerns about death, and psychosocial support for the patient and his or her caregivers, as well as management of more typical psychiatric symptoms.

The US Food and Drug Administration has approved filgrastim-sndz (Zarxio), a biosimilar of filgrastim (Neupogen), and the first such agent to be approved in the United States.

ONS has released a position paper on palliative care, emphasizing its importance throughout cancer treatment and the critical role of nurses.

An FDA advisory panel unanimously endorsed EP2006, a biosimilar of filgrastim, a biologic used to treat neutropenia caused by chemotherapy treatment.

According to three associated and recently published large randomized studies, while about 75% of cancer patients with major depression do not receive any treatment for their depression, a new system of integrating depression treatment into cancer patient care can transform patient outcomes.

Her recent history was marked by a rather rapid decline over the past 2 months. Long dormant melanoma now spread widely. Her family filled the room. She sat there, still, eyes closed, the pale yellow of advanced liver failure painted on every inch of her body.

The FDA has approved combined netupitant and palonosetron (Akynzeo) for the treatment of chemotherapy-related nausea and vomiting in patients with cancer.

Cancer patients on palliative care wards were more likely to experience a dignified death than patients in other parts of cancer centers, a recent study found.

Cognitive dysfunction during and following treatment for cancer, often referred to as “chemobrain,” is an adverse effect of cancer treatment that may interfere with patients’ ability to resume their precancer lifestyle, with subsequently reduced quality of life.

With the growing number of cancer survivors, there is increased interest in understanding and preventing post-treatment sequelae that may limit full recovery to prediagnosis health.

Much of the existing research into the phenomenon commonly referred to as “chemobrain” has been descriptive, and we know enough now to identify some patients at risk for cognitive changes after a diagnosis of cancer.

This review will focus largely on the effects of systemic cytotoxic treatment on cognitive function, reflecting what has been most extensively studied in the literature.

Results of a new study indicate that half of patients with multiple myeloma were referred to specialist palliative care.