
Laurence Albigès, MD, PhD, speaks to how patients with treatment-naïve advanced or metastatic renal cell carcinoma can benefit from treatment with nivolumab and ipilimumab.

Your AI-Trained Oncology Knowledge Connection!


Laurence Albigès, MD, PhD, speaks to how patients with treatment-naïve advanced or metastatic renal cell carcinoma can benefit from treatment with nivolumab and ipilimumab.

Patients with prostate cancer who received surgery had the highest rate of treatment-related regret followed by radiotherapy and active surveillance.

Patients with locally advanced cervical cancer did not see further benefit from the addition of concurrent durvalumab to chemoradiotherapy.

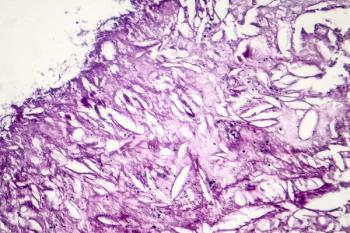
Prospective data found higher rates of occult signet ring cell gastric cancer among individuals with no family history of gastric cancer but who carried CDH1 P/LP variants.

Laurence Albigès, MD, PhD, shares updated key findings from the phase 3 CheckMate 214 trial.

Gennady Bratslavsky, MD, spoke about the evolving field of surgery for renal cell carcinoma at the 15th Annual Interdisciplinary Prostate Cancer Congress® and Other Genitourinary Malignancies.
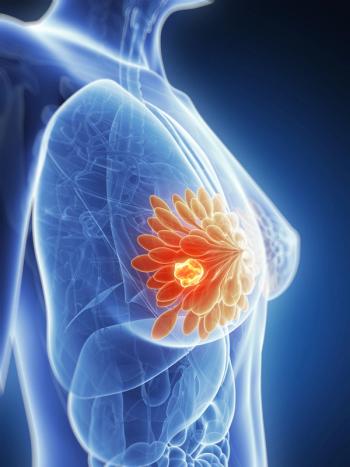
Patients with clinically lymph node–positive breast cancer who achieved cN0 disease following treatment neoadjuvant chemotherapy with 3 or more negative sentinel lymphoma nodes identified by sentinel lymphoma node biopsy alone had a decrease in nodal recurrence.

A biologics license application for sintilimab plus chemotherapy in first-line nonsquamous non–small cell lung cancer was not approved by the FDA and a complete response letter was issued to the drug developer.

Gennady Bratslavsky, MD, spoke about the evolution for treatments in renal cell carcinoma and how surgery may play a role.

Based on data from the phase 3 VISION trial, 177Lu-PSMA-617 may now be used to treat patients who were previously treated with androgen receptor pathway inhibitors plus taxane-based chemotherapy for metastatic prostate specific membrane antigen–positive castration-resistant prostate cancer.

The 6.5-year updated analysis of the phase 3 CheckMate 067 trial highlighted notable overall survival benefit with nivolumab alone or in combination with ipilimumab for patients with advanced melanoma.
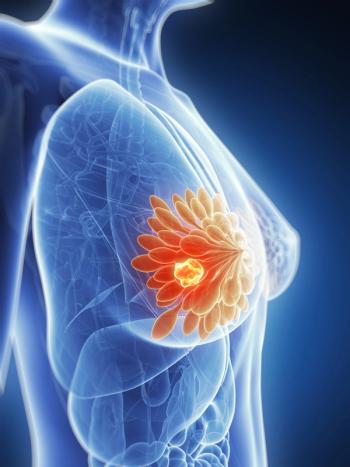
Findings from a meta-analysis indicated that pathologic complete response is a notable predictor of outcomes in HER2-positive breast cancer.
Axel Merseburger, MD, PhD, spoke about implementing the treatment combination of enzalutamide plus docetaxel/prednisone for progressive castration-resistant prostate cancer from the PRESIDE trial into the real-world.

A survey of United States breast oncologists suggested that racial differences exist in the perceived barriers to accessing genetic counseling and testing for patients with breast cancer.


Laurence Albigès, MD, PhD, speaks to the patient population included in the phase 3 CheckMate 214 trial, assessing nivolumab plus ipilimumab in patients with treatment-naïve advanced or metastatic renal cell carcinoma.
Survival among patients with multiple myeloma appears to be influenced by factors such as socioeconomic status and treatment facility type.
A survey suggests individuals with cancer who were undergoing active treatment were more likely to endorse COVID-19 related misinformation than those with no history of cancer.

Maurie Markman, MD, sits down with CancerNetwork® to discuss proposed legislation that would put a time limit on how long drugs with an accelerated approval can stay on the market, and how that may negatively impact patients with cancer.

Yelena Y. Janjigian, MD, spoke about which biomarkers were most predictive for treatment of localized gastric cancer.

Pembrolizumab has been approved by the FDA for the use in advanced microsatellite instability–high/mismatch repair–deficient endometrial cancer following prior systemic therapy.
Patients with mantle cell lymphoma appeared to benefit from brexucabtagene autoleucel as salvage therapy in the real-world setting.
7HP340 was granted fast track designation in combination with an anti–CTLA-4 treatment by the FDA for patients with unresectable or malignant melanoma for whom PD-1 inhibition therapy has failed.

For Kidney Cancer Awareness Month, CancerNetwork® spoke with Daniel M. Geynisman, MD, about how emerging data in the treatment of renal cell carcinoma stand to further impact the standard of care.

During the Association of Community Cancer Centers 48th Annual Meeting & Cancer Center Business Summit, Candice Roth, MSN, RN, CENP, spoke about electronic pathways embedded in electronic medical records.

A survival benefit was observed in patients with advanced or recurrent endometrial cancer who were treated with maintenance selinexor.

The phase 3 PRIME study showed increased progression-free survival for patients with newly diagnosed ovarian cancer who were treated with an individualized starting dose of maintenance niraparib vs placebo.

The iPocc trial indicated that patients with ovarian cancer experienced an improvement in progression-free survival when treated with intraperitoneal carboplatin plus paclitaxel compared with intravenous chemotherapy, but this benefit did not translate to overall survival.

Phase 3 SOROYA trial revealed promising response rates with mirvetuximab soravtansine in patients with platinum-resistant ovarian cancer and high folate receptor–alpha expression.

Data presented at 2022 SGO from the phase 2 OVARIO trial show promise of niraparib plus bevacizumab in high-risk ovarian cancer treated with frontline platinum-based chemotherapy.