Oncology NEWS International
- Oncology NEWS International Vol 8 No 7
- Volume 8
- Issue 7
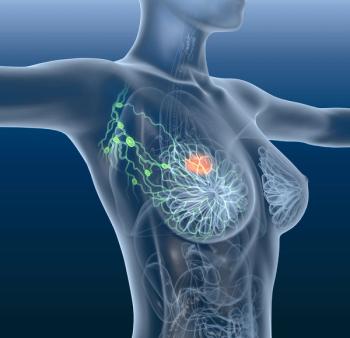
Epirubicin as Adjuvant Therapy for Breast Cancer
ASCO-Substituting epirubicin for methotrexate in a commonly used adjuvant regimen significantly increased survival for premenopausal women with node-negative early-stage breast cancer in a randomized study by the Danish Breast Cancer Cooperative Group and Swedish Oncology Centers reported at the American Society of Clinical Oncology annual meeting
ASCOSubstituting epirubicin for methotrexate in a commonly used adjuvant regimen significantly increased survival for premenopausal women with node-negative early-stage breast cancer in a randomized study by the Danish Breast Cancer Cooperative Group and Swedish Oncology Centers reported at the American Society of Clinical Oncology annual meeting.
Henning Mouridsen, MD, of Copenhagen University Hospital, reporting for the group, said, This study shows that an epirubicin-based regimen offers highly significant disease-free and overall survival advantages for premenopausal breast cancer patients compared to a cyclophosphamide, methotrexate, fluorouracil (CMF) regimen. By using the epirubicin-based regimen instead of CMF, we can decrease the risk of death from breast cancer in premenopausal women by approximately 20% to 25%.
Epirubicin is included in standard treatment regimens for breast cancer in many countries and is currently being considered for approval by the FDA. [Epirubicin recently received an FDA advisory panels recommendation for approval as adjuvant therapy.] Dr. Mouridsen said the researchers used epirubicin rather than doxorubicin because studies suggest that the two anthracyclines have similar efficacy while epirubicin is less cardiotoxic.
The study results concerning epirubi-cin will have a major impact on the management of breast cancer, Dr. Mouridsen said. Except in the United States, where epirubicin has not yet been approved, women with early breast cancer are generally treated with a regimen based on either epirubicin or methotrexate. This study shows that epirubicin may be the better treatment option for premenopausal women.
The study included 1,195 pre- and postmenopausal women with early-stage breast cancer. Following surgery, patients were randomized to intravenous CMF; intravenous CEF (cyclophosphamide, epirubicin, fluorouracil); or one of these regimens plus oral pamidronate. Median follow-up was 61 months, and 1,175 patients were evaluable. Dr. Mouridsen presented data only on the arms directly comparing CMF to CEF, without pamidronate (see Table 1).
At 6 years of follow-up, survival of premenopausal women with node-negative, grade 2-3 tumors was 93% with CEF vs 83% with CMF (P < .01, Table 2). Survival of all premenopausal patients was 76% with CEF vs 69% with CMF
(P = .01). Dr. Mouridsen said that this constituted a 23% relative reduction in mortality with CEF in premenopausal women. There was no significant advantage for CEF in the subgroup of premenopausal women with node-positive, receptor-negative or receptor status unknown tumors, nor were there significant differences between the two regimens in postmenopausal women.
Therapy was well tolerated, and doses were delivered as scheduled to 96% of women receiving CEF and to 95% of women receiving CMF. Hematologic toxicities were evenly distributed in the two groups. There were no instances of congestive heart failure or of leukemia. However, alopecia occurred in 87% of the CEF group vs only 7% in the CMF arm. Amenorrhea was induced in 80% of women on CEF vs 60% of women on CMF.
In premenopausal women, CEF is superior to CMF in terms of recurrence-free survival and overall survival, but this superiority is achieved at the cost of hair loss and loss of menstrual function, Dr. Mouridsen concluded.
During the discussion, a question arose as to whether the increased efficacy of CEF might not be attributable to the induction of early menopause. Dr. Mouridsen doubted that this was the case, since patients with and without amenorrhea achieved the same benefit with CEF as with CMF. If you look at the total population of patients with amenorrhea during treatment, they do better than patients who do not have amenorrhea, but this may also be due to an interaction with the receptor status, he said. He noted that recent data from the International Breast Cancer Study Group suggest that there is no clear effect of chemotherapy-induced amenorrhea when adjusted for node status, receptor status, and age.
Articles in this issue
over 26 years ago
Nasal Angiogenesis Inhibitor May Stop Kaposi’s Sarcomaover 26 years ago
Surgeon’s Perspective on Neoadjuvant Chemo for Breast Cancerover 26 years ago
STAR Breast Cancer Prevention Trial Begins Enrollmentover 26 years ago
Studies Suggest New Approaches in Hereditary Ovarian Cancerover 26 years ago
Lycopene Beneficial in Prostate Cancerover 26 years ago
Komen Launches REMEMBERover 26 years ago
Advice and Support for Daughters of Breast Cancer Patientsover 26 years ago
Fetus May Be Harmed by Second-Hand Smokeover 26 years ago
Genes Linked to Smoking Affinity, Smoking-Induced Lung Cancerover 26 years ago
Ultraviolet Light Slated for Review as CarcinogenNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.