Oncology NEWS International
- Oncology NEWS International Vol 9 No 2
- Volume 9
- Issue 2
Rituximab as Single Agent May Improve Response in Subset of Multiple Myeloma Patients
CLEVELAND-Rituximab (Rituxan) as a single agent appears to be active in a subset of multiple myeloma patients who have CD20+ plasma cells. That finding, reported at the ASH meeting, came as a result of a study by Mohamad A. Hussein, MD, and colleagues at the Cleveland Clinic Taussig Cancer Center to evaluate the effectiveness of rituximab in improving the response rate to melphalan/prednisone (Alkeran/Deltasone) as well as progression-free survival.
CLEVELANDRituximab (Rituxan) as a single agent appears to be active in a subset of multiple myeloma patients who have CD20+ plasma cells. That finding, reported at the ASH meeting, came as a result of a study by Mohamad A. Hussein, MD, and colleagues at the Cleveland Clinic Taussig Cancer Center to evaluate the effectiveness of rituximab in improving the response rate to melphalan/prednisone (Alkeran/Deltasone) as well as progression-free survival.
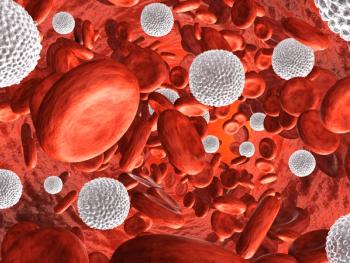
The overall survival of multiple myeloma has been minimally impacted over the past 35 years, Dr. Hussein observed. Several biologic characteristics of the disease may contribute to this failure to achieve durable remissions. Biologic factors that theoretically contribute to disease resistance include malignant plasma cells having a protected apoptotic signal, a proliferative monoclonal B cell compartment, a peripheral T cell population that is susceptible to apoptosis upon stimulation, and multi-drug resistance (MDR) gene expression, he explained.
Attractive Study Candidate
Rituximab was an attractive candidate for study because it produces antibody-dependent cell and complement mediated cytotoxicity against CD20+ cells. According to Dr. Hussein, 17% to 20% of malignant plasma cells are CD20+. The Cleveland Clinic researchers also suspect that a small proliferative CD20+ monoclonal B cell compartment could be responsible for feeding the non-proliferative myeloma compartment in plateau phase. The use of rituximab after achieving plateau phase in multiple myeloma could theoretically prevent this problem.
Pretreatment of DHL-4 B lymphoma cell lines with rituximab resulted in inhibition of cell proliferation and cell death, as well as reversal of the cell line resistance to several cytotoxic drugs, he said. This feature of the drug could enhance responses to melphalan and prednisone.
Goals and Results
This Phase II study had several goals:
evaluate the role of rituximab in improving the response rate to melphalan and prednisone;
assess the efficacy of rituximab as maintenance therapy;
determine if rituximab decreases residual disease in plateau phase;
evaluate toxicity; and
evaluate the role of rituximab in inducing apoptosis of malignant plasma cells.
The study enrolled 28 patients with newly diagnosed multiple myeloma. At the time the study was reported at the ASH meeting, 26 had completed the initial cycle of rituximab and continued to melphalan/prednisone, and 25 of those could be evaluated for response.
Patients were treated with rituximab 375 mg/m² IV weekly for 4 weeks every 6 months. Treatment continued for six cycles or until disease progression. Patients were also treated with a standard regimen of melphalan/prednisone (see Table 1).
Bone marrows were examined at diagnosis, after 1 or 2 weeks, at the end of rituximab therapy, and at the time of the plateau phase. Flow cytometry was used to examine bone marrow CD20, CD38, and CD56 expression, and peripheral blood CD19, CD20, CD56, and CD38 expression.
The first cycle of rituximab produced the following results.
2/25 patients had major responses.
2/25 had minor responses.
18/25 had stable disease.
3/25 had disease progression.
Dr. Hussein said that 4 patients with major or minor responses were all CD20+ and that 1 patient with stable disease had 7% of plasma cells co-marked with CD20.
Following a median of 5 cycles of melphalan/prednisone, there were these results.
13/25 patients (52%) had major responses.
3/25 (12%) had minor responses.
7/25 (28%) had stable disease.
2/25 (8%) had progressive disease
Mild Toxicity
Toxicity associated with rituximab was mild and included Grade 1 or 2 reactions in 15/28 patients, primarily rigors, fevers/chills, arthralgias, and local skin reactions. During melphalan/prednisone, 12/26 patients experienced grade 3/4 leucopenia and/or thrombocytopenia, resulting in therapy delay, dose reduction, or the use of growth factors.
Myelosuppression appears to be more pronounced with the combination than with melphalan/prednisone alone, Dr. Hussein commented. Rituxan as a single agent appeared to be active in a subset of MM patients, possibly in those who co-express CD20 on plasma cells. The role of rituximab in improving the response rate to melphalan/prednisone, and progression-free survival, is yet to be determined.
Articles in this issue
about 26 years ago
Neoadjuvant Docetaxel Increases Response Rate in Large Breast Tumorsabout 26 years ago
Faslodex, a Pure Antiestrogen, Shows Antitumor Activityabout 26 years ago
Tumor-Associated Proteases Predict Outcome in Node-Negative Patientsabout 26 years ago
Paclitaxel/Herceptin Effective in Metastatic Breast Cancerabout 26 years ago
Conservative Surgery Alone Not Sufficient to Prevent RecurrenceNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.