Oncology NEWS International
- Oncology NEWS International Vol 11 No 12
- Volume 11
- Issue 12
Stereotactic Radiosurgery Benefits Brain Met Patients
NEW ORLEANS-For certain types of patients with brain metastases, the addition of stereotactic radiosurgery after whole brain radiation therapy improved survival as well as local control, performance status, and steroid dependency, according to a phase III study by the Radiation Therapy Oncology Group (RTOG). Lead investigator Paul W. Sperduto, MD, of Methodist Hospital, Minneapolis, presented the results at the 44th Annual Meeting of the American Society for Therapeutic Radiation and Oncology (abstract plenary 5).
NEW ORLEANSFor certain types of patients with brain metastases, the addition of stereotactic radiosurgery after whole brain radiation therapy improved survival as well as local control, performance status, and steroid dependency, according to a phase III study by the Radiation Therapy Oncology Group (RTOG). Lead investigator Paul W. Sperduto, MD, of Methodist Hospital, Minneapolis, presented the results at the 44th Annual Meeting of the American Society for Therapeutic Radiation and Oncology (abstract plenary 5).
"We consider whole brain radiation therapy plus radiosurgery to be the new standard of care for patients who fit the eligibility for this trial," he said.
RTOG 95-08 enrolled 333 cancer patients from 34 institutions between 1996 and 2001 in a study that evaluated whether stereotactic radiosurgery improved overall survival in patients with one to three brain metastases. The study was stratified by the number of brain metastases and the extent of extracranial metastases. The patients were randomized to receive whole brain radiation therapy (WBRT) plus stereotactic radiosurgery or WBRT alone. WBRT was given at 250 cGy/fraction up to 3,750 cGy in 3 weeks. The stereotactic radiosurgery dose was based on tumor size and was delivered within 1 week of completion of WBRT.
The intention-to-treat analysis of all patients showed overall survival of 6.5 months for the WBRT plus radiosurgery patients and 5.7 months for WBRT alone (P = .13), Dr. Sperduto reported. For certain groups of patients, there was a statistically significant improvement in survival with stereotactic radiosurgery (see Table). These included patients with a solitary brain metastasis; those with one to three metastases and age less than 50; those with one to three metastases and non-small-cell lung cancer (NSCLC); and those with one to three metastases and RTOG RPA class I. [RPArecursive partitioning analysisclasses are based on Karnofsky performance status, age, control of primary tumor, and extracranial metastasis.]
For several other groups, the survival benefit approached significance. These included patients with Karnofsky performance status of 90 to 100 (10.2 vs 7.4 months for WBRT alone), patients with tumor size greater than 2 cm, and patients with a controlled primary tumor.
Dr. Sperduto speculated that the lack of an overall survival benefit with the addition of radiosurgery might be due to the high rate of patients who were randomized to radiosurgery but did not receive it19% overall and 24% with two to three metastases. Secondly, many patients in the WBRT group (17%) received salvage radiosurgery.
RPA class I patients (age less than 65, Karnofsky performance status 70 or higher, controlled primary tumor, and no extracranial metastases) had the best outcomes, with a 2-year survival of 40%, Dr. Sperduto said. Multivariate analysis found RPA class to be by far the most significant predictive factor. Components of the RPA classnamely Karnofsky performance status, age, and extracranial metastaseswere also significant prognostic factors, he said.
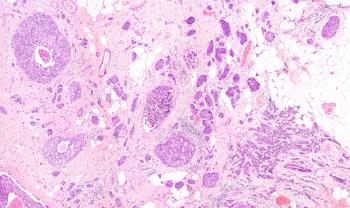
Salvage surgery (craniotomy) was performed on 4% to 5% of patients in both arms. Interestingly, pathology review showed that in the radiosurgery arm, all patients had radiation necrosis, but in the WBRT alone arm, every patient had viable tumor, he noted.
Karnofsky performance status at 6 months was more likely to be stable or improved in the radiosurgery group. Patients in the radiosurgery group were also less likely to be steroid-dependent at 6 months, to have higher tumor response rates at 3 months, and to have greater reduction of edema than patients receiving WBRT alone, Dr. Sperduto said.
The treating institutions noted local control at 1 year to be 82% for the WBRT plus radiosurgery group, compared with 71% for WBRT alone (P = .01).
Both treatments were well tolerated, with acute and late grade 3-4 toxicities less than 3% per arm. The cause of death was systemic disease in more than two thirds of patients.
Dr. Sperduto called the improvements in performance status, local control, and other quality-of-life issues "at least as important as, if not more important than," the survival benefit in some subsets of patients. Based on these findings alone, he said, "WBRT followed by stereotactic radiosurgery should become the standard of care for patients with one to three brain metastases who meet the eligibility criteria for RTOG 95-08. The survival advantage is an added benefit."
Articles in this issue
about 23 years ago
Cancer Risk From Tainted Polio Vaccine Undetermined: IOM Reportabout 23 years ago
Tailored Messages Motivate Women to Get Mammogramsabout 23 years ago
Chemo/Rituximab Is Effective as First-Line CLL Therapyabout 23 years ago
Preoperative Capecitabine/RT Downstages Rectal Cancerabout 23 years ago
Intraoperative Lymphatic Mapping Enhances Cancer Stagingabout 23 years ago
Rituximab Ups Survival in Aggressive and Indolent NHLabout 23 years ago
Genzyme Molecular Oncology Begins Kidney Cancer Vaccine Trialabout 23 years ago
Lower Breast Cancer Survival in Hispanics: New Mexico Studyabout 23 years ago
Concurrent Chemo/RT More Likely to Save LarynxNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.