Treatment with Cisplatin-Based Chemotherapy Yields High Risk of Mortality Unrelated to Disease in Testicular Cancer
Patients with testicular cancer who are treated with platinum-based chemotherapy or radiotherapy have an increased risk of mortality unrealted to their disease.
The use of platinum-based chemotherapy (PBCT) or radiotherapy resulted in an increased risk of death, and more than 2 cycles of cisplatin-based chemotherapy yielded the emergence of increased risks among those with testicular cancer after more than 10 years of follow-up, according the results of a study published in the Journal of Clinical Oncology.
The overall excess of deaths that were reportedly unrelated to testicular cancer was 23% (standardized mortality ratio [SMR], 1.23; 95% CI, 1.14-1.33; absolute excess risk [AER], 11.14) compared with the general population. Increased risks were reported following PBCT (SMR, 1.23; 95% CI, 1.07-1.43; AER, 7.68). Patients with the highest non–testicular cancer mortality were those with less than 20 years since their diagnosis (SMR, 2.27; 95% CI, 1.32-3.90; AER, 14.42). The overall incidence of noncancer mortality increased by 15%, according to investigators (SMR, 1.15; 95% CI, 1.04-1.27; AER, 4.71).
“We hypothesize that cytotoxic treatment is the main risk factor for increased mortality. The increased mortality risk might be reduced by lifestyle improvements, which should be recommended following TC [testicular cancer] treatment,” the investigators wrote.
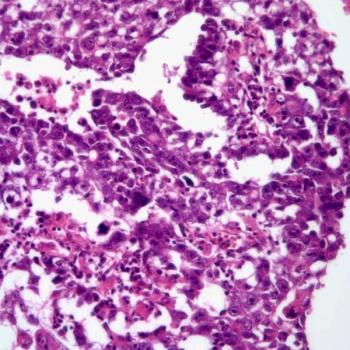
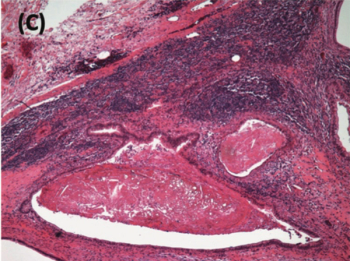
A total of 5707 patients were enrolled on the study, with a median follow-up time of 18.7 years; notable, the median follow up was greater than 20 years for 46% of participants. At the time of diagnosis, the median patient age was 33.1 years (interquartile range [IQR], 27.2-40.8). During follow-up, 15% (n = 846) of patients had died, with testicular cancer being the cause for 3.2% (n = 181) and 82% of patients dying during the first 5 years. A total of 12% (n = 665) of patients died from causes other than testicular cancer, with a median follow-up time of 17.7 years (IQR, 10.3-24.7). At the time of diagnosis, the median age was 44.6 years and 67% of patients had seminoma histology.
Investigators reported that the 25-year crude cumulative mortality unrelated to testicular cancer was 13.7% (95% CI, 12.5%-14.9%), and the population expected (PE) risk was 11.3%. Moreover, after patients received surgery, the cumulative risk of non–testicular cancer mortality was 10.1% (95% CI, 8.0%-12.4%; PE risk, 10.6%), as well as being 9.5% after treatment with PBCT (95% CI, 7.9%-11.3%; PE risk, 8.1%) and 19.0% (95% CI, 16.8%-21.2%; PE risk, 14.9%) after radiotherapy. Additionally, patients who received PBCT and radiotherapy had a non-disease mortality risk of 18.4% (95% CI, 13.3%-24.2%; PE risk, 14.1%).
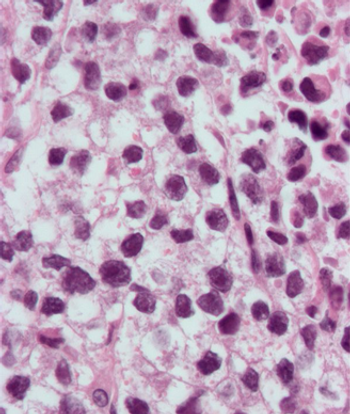
Second cancers unrelated to testicular cancer were the cause of death in 4.5% (n = 257) patients, translating to a 53% excess in the general population (SMR, 1.53; 95% CI, 1.35-1.73). A significant 1.43- to 3.24-fold increase in mortality related to a second cancer emerged following treatment with PBCT, radiotherapy, and PBCT plus radiotherapy. Treatment with PBCT was found to be associated with a 1.69- to 6.82-fold increase in excess mortality due to second cancers such as disease of the lip, oral cavity, pharynx, esophagus, lung, bladder, and leukemia. Patients who received radiotherapy experienced a 3.02- to 4.91-fold increase in excess mortality for diseases of the lip, oral cavity, pharynx, stomach, liver, pancreas, and bladder.
Investigators identified that patients who were older at diagnosis had a decreased SMRs for second cancer mortality. For patients who were younger than 20 years of age, the SMR was 3.68 (95% CI, 1.19-11.40). Additionally, those between the ages of 20 to 30 years old had an SMR of 2.00 (95% CI, 1.28-2.99) and those greater than 50 years had an SMR 1.28 (95% CI, 1.04-1.57).
A total of 7.1% (n = 408) of patients died from non-cancer causes; this was 15% higher than the general population (SMR 1.15; 95% CI, 1.04-1.27). The overall noncancer mortality for the 3 treatment types was 1.17- to 1.55-fold higher than expected.
Following surgery, the risk of death from infectious disease was 3.73-fold higher. Investigators also identified an association between a 3.29-fold increase of mortality due to diseases of the genitourinary system and treatment with PBCT. Additionally, investigators reported that a 1.65-fold increase in suicide compared with the general population appeared to be associated with treatment with PBCT. Patients who received radiotherapy had a 2.46-fold increased risk of mortality due to diseases of the digestive system.
Although increased mortality due to heart disease was noted among those who were treated with PBCT and radiotherapy, overall death due to cardiovascular disease was not found to increase in the overall study population. Conversely, death related to cardiovascular disease in the first year of follow-up was found to significantly increase among those who received treatment with PBCT (SMR, 3.90; 95% CI, 1.26-12.08; AER, 10.42). Three patients died, including 2 who died due to acute myocardial infractions and 1 from stroke.
Reference
Hellesnes R, Myklebust TÅ, Fosså SD, et al. Testicular cancer in the cisplatin era: causes of death and mortality rates in a population-based cohort. J Clin Oncol. Published Online August 13, 2021. doi:10.1200/JCO.21.00637
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.