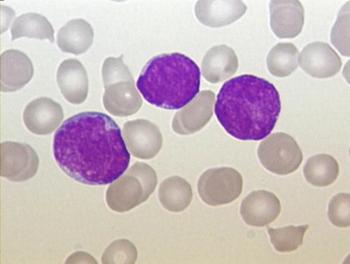
Leukemia
Latest News

Latest Videos
CME Content
More News

The panelists conclude their discussion by offering future perspectives on CLL treatment, emphasizing remaining areas of unmet needs in the treatment landscape.

A panel of oncology experts discuss recent advancements surrounding novel therapies for CLL, exploring their potential impact on future treatment paradigms.
Measurable residual disease–guided ibrutinib plus venetoclax in chronic lymphocytic leukemia appears to be particularly beneficial in patients with unmutated IGHV and specific genetic abnormalities.
Rachel Rau, MD, gives her perspective on the use of asparaginase treatments for pediatric patients with acute lymphocytic leukemia.

Sameer A Parikh, MD, leads an expert discussion regarding emerging resistance data and its potential impact on treatment sequencing.

Sikander Ailawadhi, MD, review real-world data findings recently presented at ASH 2023, highlighting their potential implications on the treatment landscape.
Administering pegylated asparaginase continuously to pediatric patients with acute lymphoblastic leukemia appears to be safe without compromising the efficacy of treatment.
HEMO-CAR-T can now proceed with its evaluation as a treatment for those with acute myeloid leukemia as part of a phase 1 trial.

Vanderbilt University Medical Center and Winship Cancer Institute at Emory University Face Off on recent data in multiple myeloma and acute lymphoblastic leukemia.

Investigators discontinued the phase 3 ENHANCE-3 study after magrolimab plus azacitidine and venetoclax yielded an increased risk of death in those with acute myeloid leukemia.

The FDA sets a Prescription Drug User Fee Action date of June 21, 2024 for blinatumomab as a treatment for those with CD19-positive B-cell precursor acute lymphoblastic leukemia.

A panel of oncology experts review meta-analysis data evaluating bleeding risk with covalent BTKis, discuss the impact of these data on treatment decision making, and explore strategies in managing BTKi-related bleeding risk.

Sikander Ailawadhi, MD, offers expert insight into managing the risk of atrial fibrillation in CLL patients receiving BTKis.

Most patients with acute myeloid leukemia appear to remain on treatment with ziftomenib plus standard-of-care therapy in the phase 1 KOMET-007 trial.

Amber Koehler, PA-C, provides expert perspective on addressing hypertension risk in CLL patients undergoing treatment with BTK inhibitors.

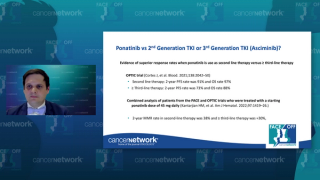
A panel of oncology experts offer insights into key consideration factors for BTKi selection for CLL in the relapsed and refractory setting, exploring the impact of emerging MAIC data on treatment decision making.

A panel of oncology experts review recently presented data updates from ALPINE and ELEVATE-RR, discussing the potential impact of these findings on the clinical practice setting.

A panel of oncology experts share their general approach in navigating treatment selection for patients with R/R CLL, highlighting key factors to consider in making treatment decisions.
The FDA sets a Prescription Drug User Fee Action Date of November 16, 2024 for obe-cel as a treatment for those with relapsed/refractory B-cell acute lymphoblastic leukemia.

PTX-252 incorporates a novel molecular entity designed to enhance how cancer cells respond to chemotherapy.

Expert faculty highlight key updates from trials evaluating combination therapy approaches using venetoclax plus a BTKi in the frontline setting.
Findings from a phase 1a/1b trial highlight that treatment with NX-5948 appears to be tolerable among patients with relapsed/refractory B-cell malignancies.

A panel of experts discuss the role of fixed duration therapy with venetoclax and obinutuzumab, outlining their general approach for patient selection.

Investigators report favorable overall survival among patients with chronic lymphocytic leukemia who receive ibrutinib/venetoclax over FCR.
Ghayas C. Issa, MD, gave an all-encompassing review of current treatment options for acute myeloid leukemia and what to expect in the future.