
Results reported at the 2021 ASCO Annual Meeting show that half of patients treated in the FORWARD II trial achieved a response to therapy with mirvetuximab soravtansine and bevacizumab.

Your AI-Trained Oncology Knowledge Connection!


Results reported at the 2021 ASCO Annual Meeting show that half of patients treated in the FORWARD II trial achieved a response to therapy with mirvetuximab soravtansine and bevacizumab.
Across 3 health-related quality of life scales, the combination of pembrolizumab plus lenvatinib had similar or better outcomes than sunitinib for patients with metastatic renal cell carcinoma receiving treatment in the frontline.
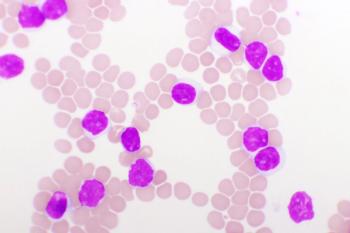
While survival rates were similar, acalabrutinib had lower rates of atrial fibrillation and other adverse events than ibrutinib for previously treated CLL.
Data from 2 clinical trials proved that larotrectinib is efficacious and safe in treating adults and children with NTRK fusion-positive central nervous system cancers.
Evidence of preliminary activity was noted with the use of the RET inhibitor selpercatinib in pediatric patients with solid tumors harboring RET alterations.
The addition of neoadjuvant nivolumab plus platinum-doublet chemotherapy significantly improved pathological complete response rates and showed a greater depth of pathological response compared with chemotherapy alone in patients with resectable non–small cell lung cancer.

In a first-in-human study of patients with relapsed or refractory multiple myeloma, the autologous CAR T-cell therapy CART-bbBCMA led to at least a partial response in all treated patients.
Patients with early-stage breast cancer who have ultralow risk disease indicated by a 70-gene signature demonstrated an excellent survival prognosis regardless of clinical risk.
With further follow-up, lifileucel (LN-144) continued to show durable responses in patients with heavily pretreated advanced or metastatic melanoma who have progressed on multiple therapies, including prior anti–PD-1/PD-L1 therapy
In an updated analysis of the combination of lenvatinib and pembrolizumab for patients with advanced melanoma efficacy results continue to show a durable response.
Nivolumab monotherapy, or in combination with ipilimumab, continued to demonstrate durable improvements in overall survival compared with ipilimumab alone in patients with previously untreated advanced melanoma.

Phase 2 results presented during the 2021 ASCO Annual Meeting suggest durvalumab plus chemotherapy as neoadjuvant therapy for triple-negative breast cancer may be beneficial in certain patients.
Although adjuvant treatment with gefitinib delayed early relapse in patients with completely resected EGFR-mutant non–small cell lung cancer, the agent did not significantly improve disease-free survival or overall survival compared with cisplatin/vinorelbine.
With a de-escalation strategy for administration of trastuzumab and pertuzumab in the neoadjuvant setting, patients with HER2-positive, hormone receptor–negative breast cancer experienced high rates of response and survival.

Patients with platinum-pretreated EGFR exon 20 insertion mutation–positive metastatic non–small cell lung cancer experienced antitumor activity with oral TKI mobocertinib, according to results presented at the 2021 ASCO Annual Meeting.
About 40% of patients who progressed on placebo following resection of melanoma experienced an objective response with crossover to pembrolizumab in the phase 3 EORTC 1325/KEYNOTE-054 trial.
Results of a phase 1/2 trial presented at the 2021 ASCO Annual Meeting show the feasibility of an approach targeting CLL-1 cells in pediatric patients with relapsed or refractory acute myeloid leukemia.
CancerNetwork® sat down with Larry Anderson, MD, PhD, at the 2021 ASCO Annual Meeting to talk about updated data from the KarMMa trial of CAR T-cell therapy idecabtagene vicleucel to treat patients with relapsed or refractory multiple myeloma.

Updated data from the pivotal L-MIND trial that were presented at the 2021 ASCO Annual Meeting continue to support the use of tafasitamab-cxix in patients with relapsed/refractory diffuse large B-cell lymphoma.
The novel combination of polatuzumab vetodin, rituximab and lenalidomide improved overall response and complete response for patients with relapsed/refractory diffuse large B-cell lymphoma.

Compared with immediate prior therapy, selpercatinib resulted in a greater proportion of objective responses in patients with non–small cell lung cancer whose tumors harbor RET fusions.
A higher overall response rate was noted with lifileucel and pembrolizumab versus pembrolizumab alone in patients with checkpoint inhibitor–naïve advanced melanoma, according to phase 2 trial results that were reported at the 2021 ASCO Annual Meeting.
Most patients with either mantle cell lymphoma or chronic lymphocytic leukemia who were treated in a phase 1/2 trial had a response to therapy with the combination of cirmtuzumab plus ibrutinib.
Pralsetinib was well tolerated, while demonstrating robust and durable anti-tumor activity when treating heavily pretreated patients with multiple RET fusion–positive advanced solid tumors.

The phase 3 ANDROMEDA trial demonstrated positive efficacy and safety data in the treatment of newly diagnosed light chain amyloidosis.
Venetoclax plus fulvestrant did not result in better outcomes compared to fulvestrant alone in previously treated patients who had locally advanced or metastatic estrogen receptor–positive, HER2-negative breast cancer.

Palbociclib plus fulvestrant maintained a clinically meaningful overall survival improvement compared to placebo plus fulvestrant after a median follow-up of 73.3 months in patients with HR-positive, HER2-negative advanced breast cancer.
TG-1701 elicited promising clinical and pharmacodynamic activity across doses in patients with B-cell malignancies.
The combination of mosunetuzumab plus polatuzumab vedotin showed positive efficacy and safety data in a phase 1b study of patients with B-cell non-Hodgkin lymphoma.

Patients with platinum-sensitive recurrent ovarian cancer treated with niraparib had an acceptable safety profile regardless of the dose being adjusted for weight.