Wayne A. Marasco, MD, PhD, stated that by targeting 2 molecules instead of 1, higher levels of tumor cell killing can be achieved in patients with clear cell renal cell carcinoma.

Your AI-Trained Oncology Knowledge Connection!

Wayne A. Marasco, MD, PhD, stated that by targeting 2 molecules instead of 1, higher levels of tumor cell killing can be achieved in patients with clear cell renal cell carcinoma.

Leading experts in the breast cancer field highlight the use of CDK4/6 inhibitors, antibody-drug conjugates, and other treatment modalities.

Panelists discuss the need for consolidation and maintenance strategies following chimeric antigen receptor (CAR) T-cell therapy in patients with high-risk multiple myeloma, highlighting emerging real-world and clinical evidence supporting the use of agents like lenalidomide and bispecific antibodies to extend disease control and improve outcomes in those with historically shorter remissions.

Panelists discuss real-world evidence showing that chimeric antigen receptor (CAR) T-cell therapy is safe and effective in traditionally excluded populations with multiple myeloma, including those with comorbidities or central nervous system (CNS) involvement, emphasizing the role of multidisciplinary care, proactive toxicity management, and growing confidence in extending access to high-risk patients.
The Q-TWiST analysis from the LITESPARK-005 trial showed statistically significant improvement of belzutifan over everolimus in patients with clear cell RCC.
Results from a Q-TWiST analysis of the LITESPARK-005 trial showed a trend favoring belzutifan over everolimus for patients with clear cell RCC.

This is an actor portrayal of a hypothetical patient profile developed for educational purposes based on characteristics of patients with multiple myeloma as seen in clinical practice. The hypothetical case was co-developed by staff medical writers with Cancer Network/ONN.

Panelists discuss evolving frontline treatment strategies for metastatic melanoma, emphasizing recent clinical updates—particularly 4-year data from the RELATIVITY-047 trial—and exploring how these findings, including the benefits of nivolumab plus relatlimab, inform real-world decision-making for complex cases like BRAF-mutant disease with high tumor burden.

Panelists discuss how managing amivantamab-related adverse events like leg edema requires understanding of underlying mechanisms (hypoalbuminemia) and may benefit from albumin infusion, dose holds, or consultation with specialists for severe cases like infected scalp wounds.
Panelists discuss how real-world outpatient talquetamab data from Mayo Clinic show that 85% of patients can start treatment as outpatients with about 50% completing the entire step-up process without hospitalization, while different centers are developing varying approaches to cytokine release syndrome (CRS) management—from no prophylaxis with 50% admission rates to prophylactic tocilizumab with 3% admission rates—suggesting that practice preferences may ultimately determine which bispecific agents are favored based on factors like median time to CRS onset.

Panelists discuss how the 5-year data from CARTITUDE-1 demonstrate that a substantial subset of patients achieved long-term remission, suggesting a potential shift toward curative therapy.

Panelists discuss how safety outcomes from CARTITUDE-1 revealed that most adverse effects, including cytokine release syndrome (CRS) and neurotoxicity, were manageable and reversible, even in advanced-stage patients.

Panelists discuss how the COCOON study's advanced dermatologic prophylaxis protocol, including systemic antibiotics and topical treatments, can reduce skin toxicities by 50% in patients receiving amivantamab plus lazertinib therapy.
Panelists discuss how outpatient administration of talquetamab is becoming more feasible with proper patient selection, noting that although there are few absolute medical contraindications to bispecifics, they exercise caution in patients with dialysis dependency (due to different pharmacokinetics), spinal cord compression (due to inflammatory response concerns), decompensated heart failure, or active infections, while emphasizing that most myeloma patients who desire continued therapy should not be denied bispecific treatment.

With the recent approvals of T-DXd and Dato-DXd, the care for breast cancer continues to evolve and expand.

Erika Hamilton, MD, gave an overview of evolving therapies and recent trial updates for patients across breast cancer subtypes.

Combining ADCs has shown a potential improvement in survival, but it may also come with increased toxicities.

Cross-resistance makes it important to determine sequencing options across antibody-drug conjugates for patients with breast cancer.

Patients with node-negative disease who are older and have comorbidities may not be suitable to receive CDK4/6 inhibitors.

Panelists discuss management strategies for a patient with low-risk myelodysplastic syndrome with erythropoiesis-stimulating agent (ESA) failure, weighing options between initiating luspatercept or escalating ESA dosage while emphasizing the need for thorough evaluation of reversible causes before advancing therapy.
Panelists discuss how talquetamab’s unique targeting mechanism offers significant advantages for patients with prior T-cell therapy exposure, whereas future research should focus on combination strategies and understanding primary resistance mechanisms.

Panelists discuss a complex case of lower-risk myelodysplastic syndrome in a patient with rheumatoid arthritis, debating immediate transfusion for symptom relief vs thorough evaluation and targeted long-term anemia management to balance comorbidities and optimize outcomes.

An observed carryover effect with CDK4/6 inhibitors may reduce the risk of recurrence years after a patient stops treatment.

In a discussion at IBC East, Heather McArthur, MD, highlighted how immunotherapy is being utilized for patients with early-stage breast cancer.
Panelists discuss how 4-drug regimens anchored by CD38 antibodies are becoming the standard of care in myeloma, with future directions focusing on integrating novel immunotherapies and potentially redefining the role of transplant.
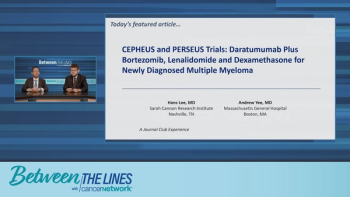
Panelists discuss that Dara-VRD offers significant benefits in sustained minimal residual disease (MRD) negativity and progression-free survival with a manageable safety profile, emphasizing dose adjustments and supportive care to balance efficacy and toxicity in frontline multiple myeloma treatment.

Panelists discuss emerging strategies to manage delayed neurotoxicity from chimeric antigen receptor (CAR) T-cell therapy in multiple myeloma, highlighting the predictive value of postinfusion lymphocyte expansion, the potential of early dexamethasone intervention, and the need for continued research and collaboration to refine toxicity prevention and ensure safer, broader use of CAR T in earlier treatment lines.
Panelists discuss recent data showing that sustained minimal residual disease (MRD) negativity strongly predicts long-term progression-free survival (PFS) in multiple myeloma, regardless of whether patients receive a 4-drug daratumumab-based regimen or standard-drug therapy, emphasizing MRD negativity as a key surrogate end point; they also highlight challenges in predicting who benefits most from intensive therapy and the importance of individualized dosing strategies to balance efficacy and tolerability across different patient populations.

Panelists discuss the growing support for incorporating chimeric antigen receptor (CAR) T-cell therapy earlier in the multiple myeloma treatment pathway, emphasizing the importance of timely referral and personalized decision-making to maximize patient outcomes before disease progression or comorbidities limit eligibility.

Heather McArthur, MD, spoke about the use of CDK4/6 inhibitors in the adjuvant setting for patients with HR+/HER2– breast cancer.