BST02 Receives FDA Fast Track Designation in Liver Cancer Management
Investigators are assessing the safety, tolerability, and initial efficacy of BST02 in those with advanced or metastatic liver cancer as part of a phase 1 trial.
Developers are assessing the safety, tolerability, and preliminary efficacy of BST02 in patients with locally advanced or metastatic liver cancer in an investigator-initiated phase 1 trial (NCT06173726).
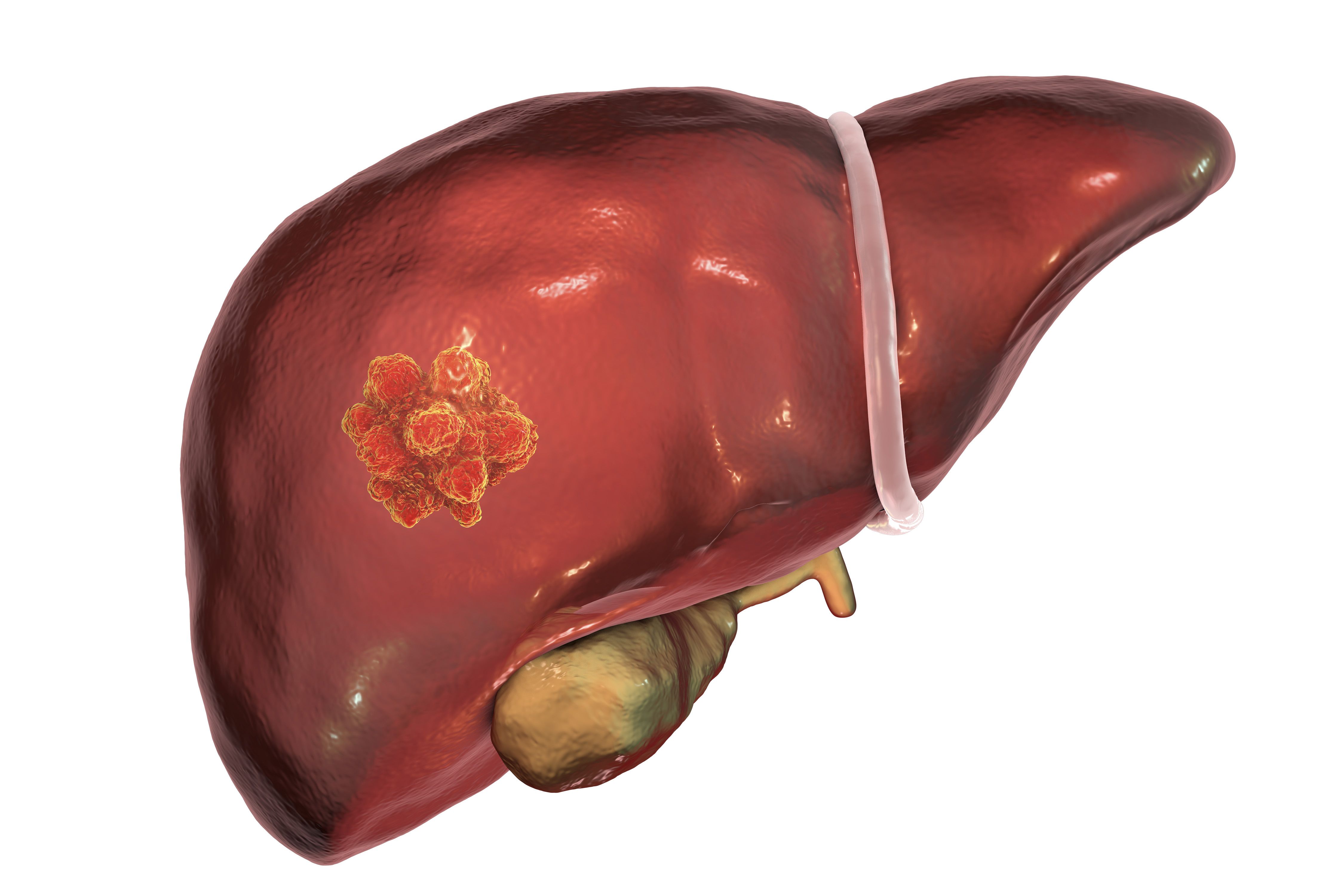
The FDA has granted fast track designation to the investigational T-cell therapy BST02 as a treatment for patients with liver cancer, according to a press release from Biosyngen.1
The regulatory agency’s designation for the investigational agent extends to all types of liver cancer, which includes those with hepatocellular carcinoma (HCC) and cholangiocarcinoma. Compared with other tumor-infiltrating lymphocyte (TIL)–based therapies, BST02 is believed to alleviate distance restrictions with its cryopreserved form and reduce the need for high interleukin-2 (IL-2) doses.
Previously, the FDA cleared an investigational new drug (IND) application for the evaluation of BST02 as a treatment for those with liver cancer as part of a phase 1/2 trial in October 2023.2 Additionally, the China National Drug Administration’s Center for Drug Evaluation approved the agent in January 2024.1 According to the press release, these designations mark BST02 as the first TIL cell therapy in the management of liver cancer to advance to the clinical stage on an international scale.
Michelle Chan, co-founder and chief executive officer at Biosyngen, “expressed gratitude” for the FDA’s fast track designation and stated that her company was committed to “advancing cell therapy for cancer globally and providing innovative treatment solutions for diverse patient populations.”1 Moreover, she underscored that developers aim to leverage their “advanced technology platforms to offer more effective and accessible treatment options for patients worldwide.”
Developers are assessing the safety, tolerability, and preliminary efficacy of BST02 in patients with locally advanced or metastatic liver cancer in an investigator-initiated phase 1 trial (NCT06173726). The study will include a dose-escalation and dose-expansion portion to determine how different IL-2 injection doses impact the efficacy and safety of BST02 in the aforementioned population.
Before administering BST02 as an injection, investigators will treat patients with cyclophosphamide at 250 mg or 1.5 g/m2 as a single intravenous infusion.
The trial’s primary end point is the occurrence and incidence of adverse effects (AEs). Other primary end points include serious AEs and dose-limiting toxicities.
Patients 18 to 75 years old with histologically or cytologically confirmed locally advanced or metastatic liver cancer—including those with stage B or C HCC and cholangiocarcinoma not suitable for local treatment based on Barcelona Clinic Liver Cancer criteria—are able to enroll on the trial. Additional eligibility criteria include having at least 1 operation without radiation or other local treatment within 4 weeks of entry to remove the tumor lesion, 1 or more measurable lesions based on RECIST v1.1 guidelines, an ECOG performance status of 0 or 1, a Child-Pugh cirrhosis score of no higher than 7 points, and a life expectancy of at least 3 months. Patients are also required to have adequate organ and bone marrow function within 2 weeks before TIL sampling to enroll.
Those with prior organ transplantation or hematopoietic stem cell transplantation or treatment with immunosuppressive agents within 4 weeks prior to tumor tissue sampling are ineligible to enroll on the trial. Patients are also unsuitable for enrollment if they have received a live vaccine within 3 months of screening or prior major surgery within 4 weeks before entry.
Previously, the FDA granted fast track designation to Biosyngen’s first-in-class immunotherapy BRG01 as a treatment for those with relapsed or metastatic nasopharyngeal carcinoma in July 2023.3 The modified T-cell therapy was designed to expand ex vivo and bind to specific antigens on cancer cells following intravenous administration, thereby mediating the killing of tumors.
References
- Biosyngen announces FDA fast track designation for BST02 in treatment of liver cancer. News release. Biosyngen. February 1, 2024. Accessed February 2, 2024. http://tinyurl.com/58am9uah
- Biosyngen's BST02, the world's first TIL therapy for liver cancer, is granted an IND approval by FDA. News release. Biosyngen. October 26, 2023. Accessed February 2, 2024. http://tinyurl.com/532trzx9
- Biosyngen's first-in-class cell therapy BRG01 receives FDA fast track designation. News release. Biosyngen. July 12, 2023. Accessed February 2, 2024. http://tinyurl.com/mr96h4ka
Adapting to a Robotic Workstation for Image-Guided Liver Cancer Surgery
December 4th 2023Govindarajan Narayanan, MD, speaks to the potential time-saving advantages of using the Epione robot for microwave ablation, cryoablation, and other surgical strategies in patients with liver cancer and other tumors.