Oncology NEWS International
- Oncology NEWS International Vol 4 No 5
- Volume 4
- Issue 5
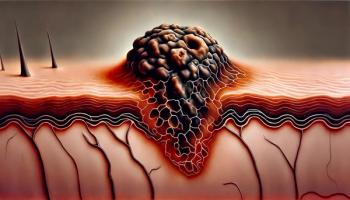
Cancer Vaccine Made From Purified Tumor Antigen Enters Phase III Melanoma Trials
NEW YORK--A mollusk protein turned out to be the best carrier for a cancer vaccine being developed by Philip O. Livingston, MD, at Memorial Sloan-Kettering Cancer Center. This approach to augmenting the immunogenicity of the GM2 ganglioside tumor antigen is about to be tested in phase III randomized trials of melanoma patients who are free of detectable disease after surgery but are at high risk for recurrence.
NEW YORK--A mollusk protein turned out to be the best carrierfor a cancer vaccine being developed by Philip O. Livingston,MD, at Memorial Sloan-Kettering Cancer Center. This approach toaugmenting the immunogenicity of the GM2 ganglioside tumor antigenis about to be tested in phase III randomized trials of melanomapatients who are free of detectable disease after surgery butare at high risk for recurrence.
The trials will also test Dr. Livingston's long-held belief thatpurified antigens, not whole tumor cells, offer the most efficientmethod of immunization.
The new cancer vaccine combines the mollusk-derived keyhole limpethemocyanin (KLH) molecule, a highly immunogenic carrier protein;saponin fraction QS-21, a potent immunological adjuvant purifiedfrom tree bark; and the GM2 ganglioside, a glycolipid found onthe cell surface of tumors of neuroectodermal origin, includingmelanoma, sarcoma, and neuroblastoma.
'A Sea of Cytokines'
Use of this vaccine will create a "sea of cytokines,"Dr. Livingston said at an international symposium on cancer vaccinessponsored by the Cancer Research Institute. The KLH will be brokendown by dendritic cells and macrophages into thousands of epitopes,recognized by thousands of T cells. The cytokines stimulated bythe vaccine will change as the immune response progresses frominitial recognition to maturation, releasing a "flood ofcytokines appropriate for each particular phase of the immuneresponse against the core antigen (GM2)," Dr. Livingstonsaid.
The cancer vaccines Dr. Livingston has been working on are designedto take the tumor au-toantigens out of their normal cell environmentand put them in the context of foreign antigens.
"Tumor antigens are poor antigens because they are autoantigens,slightly modified, and because they are surrounded by autoantigensmuch like the rest of our normal antigens," he said. "Butthe antigens of various infectious disease are surrounded by otherhighly foreign antigens--and it seems as though the immune systemhas been designed to take advantage of this difference."
The phase III randomized Intergroup trials, to be conducted bythe Eastern Cooperative Oncology Group (ECOG), will be the latestin a long series of trials that began in 1975 with studies ofmelanoma patients by Dr. Livingston and his colleagues Drs. LloydOld and Herbert Oettgen.
The researchers set out to create a vaccine that would enhancethe immunogenicity of any of a variety of tumor antigens. Initialstudies using whole cell vaccines showed no impact on any T cellactivity. "Though many patients made antibody responses,only a few were against tumor antigens. The antigen recognizedmost frequently was the ganglioside GM2. But if we injected GM2alone, we got no antibody response," he said.
The researchers found that the immunogenicity of GM2 could beincreased by adherence to the surface of BCG. This vaccine (GM2/BCG)resulted in production of moderate titer, short-lived IgM antibodiesin 86% of patients, but only occasional IgG antibody response.The improved IgM response was consistently associated with improveddisease-free and overall survival. The next step was to find amore potent carrier and adjuvant.
The long series of trials concluded with the most recent encouragingresults comparing a vaccine made from carrier KLH, adjuvant QS-21,and GM2 with the previous vaccine constructs.
Among 36 patients immunized with GM2-KLH + QS-21, 34 had increasedIgM antibody responses and 33 had increased IgG response, comparedwith 8 and 1, respectively, of 110 patients immunized with wholemelanoma cells and various adjuvants, and 70 and 16, respectively,of 82 patients immunized with GM2/BCG.
Dr. Livingston hopes that the multicenter trials, which will beginthis year, will establish whether the induction of antibodieswill have an impact on preventing melanoma recurrences.
Articles in this issue
almost 31 years ago
Genetic Therapy Gets NIH Patentalmost 31 years ago
Fusion Product Delivers Potent Toxin to Malignant Cellsalmost 31 years ago
Retinoic Acid May Enhance Chemo In Ovarian Ca Cellsalmost 31 years ago
Compounds Block ras Gene Function Compounds Block ras Gene Functionalmost 31 years ago
Companies Merge to Form NeXstaralmost 31 years ago
Antiangiogenesis Tested in Pediatric Tumorsalmost 31 years ago
Delivery of Effective Cyclophosphamide Metabolite Could Reduce Toxicityalmost 31 years ago
New Director Attends Office of Alternative Medicine Advisory Meetingalmost 31 years ago
Worksite Cancer Screening Boosts Employee MoraleNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.