- ONCOLOGY Vol 12 No 8
- Volume 12
- Issue 8
Controversies in the Management of Stage I Seminoma
Current controversies in the treatment of stage I seminoma center on the relative roles of surveillance, adjuvant radiotherapy (RT), and adjuvant single-agent chemotherapy. Surveillance has been studied in over 800 patients,
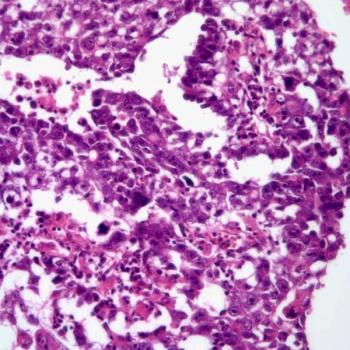
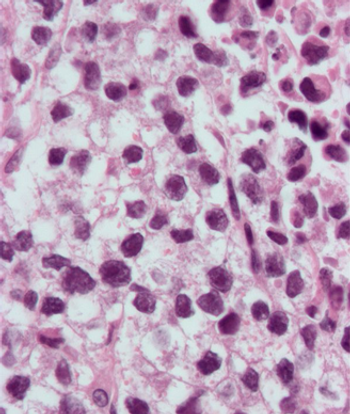
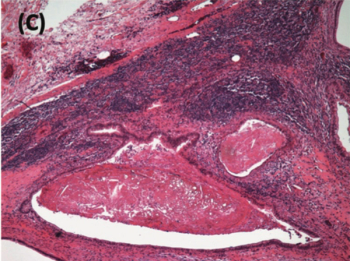
Testicular cancer is one of the therapeutic triumphs of the 20th century. Long before cisplatin (Platinol) was first used in patients with testicular cancer, radiation therapy was the standard treatment for patients with seminoma. The noted sensitivity of seminoma to radiation led to its routine use, even in advanced disease. Most patients with stage II disease (and, as mentioned by Fiveash and Sandler, even some patients with stage I disease) received prophylactic mediastinal radiotherapy.
With the advent of cisplatin-based combinations for nonseminomatous germ cell tumors, chemotherapy also proved successful in treating metastatic seminoma. Numerous studies have suggested that seminoma may be even more chemosensitive than is nonseminoma when compared stage for stage. Consequently, the newer international staging system does not consider any patient with seminoma to have advanced (or "poor-risk") disease.
Despite these successes, several unresolved issues remain in the treatment of seminoma, particularly in early-stage disease. This article does a fine job of outlining these issues and presenting a balanced discussion of the treatment alternatives.
Radiation Therapy: Balancing the Risks vs Benefits
In large part, this article balances the sins of omission with the sins of commission. Phrased more specifically, it seeks to answer the question, does radiation therapy potentially cause as many problems as it solves? To clarify this issue, it is useful to delineate the natural history of clinical stage I seminoma.
Several published series of surveillance conducted in patients with stage I seminoma report relapse rates of approximately 17% (as shown in the authors Table 2), with a range of 8.7% to 33%. Thus, if all patients with clinical stage I were given prophylactic adjuvant chemotherapy, over 80% would receive such therapy needlessly.
The same argument can be made against the need for primary retroperitoneal lymph node dissection in patients with stage I nonseminomatous germ cell tumors. A principal difference between these two local treatment approaches is that long-term toxicity is not commonplace in patients undergoing retroperitoneal lymph node dissection.
Both retroperitoneal lymph node dissection and radiation therapy are associated with morbidity in patients with early (stage I) testicular cancer. In large part, the side effects of retroperitoneal lymph node dissection are apparent shortly after the procedure. One of the principal toxicities, retrograde ejaculation, has been largely abrogated by the use of nerve-sparing dissections. This approach still entails the potential risk (albeit small) of complications from anesthesia and necessitates recovery from surgery. Other long-term complications are infrequent.
In contrast, radiation therapy to the peri-aortic lymph nodes has relatively few short-term complications but a certain risk for long-term complications, such as secondary malignancies, infertility, and cardiovascular events.
Treatment Alternatives for Early-Stage Disease
In both seminoma and nonseminoma, the success of cisplatin-based combination chemotherapy has provided a "safety net" that has enabled researchers to explore treatment alternatives for early-stage disease. Modifications in systemic therapy have been a product of numerous prospective, randomized trials, which have extended our understanding of the optimal and minimal therapy needed to achieve high cure rates in patients with disseminated disease. In the last few years, several trials have shown that there is a minimal threshold that must be crossed in order to achieve therapeutic success.
For example, prospective, randomized trials have demonstrated that lowering the dose of cisplatin is associated with a worse outcome. Also, when three cycles of cisplatin and etoposide are given rather than the three-drug combination of bleomycin, etoposide, and Platinol (BEP), the omission of bleomycin is associated with a decrease in relapse-free survival. Finally, the substitution of carboplatin (Paraplatin) for cisplatin in combination regimens also has been shown to worsen therapeutic outcome.
In summary, these trials have suggested that the minimal therapy for patients with favorable-prognosis disseminated germ cell tumors is three cycles of BEP or four cycles of cisplatin plus etoposide.
Some of the same questions about modifying therapy surround the management of stage I seminoma. As Fiveash and Sandler point out, these issues relate to radiation doses and fields, surveillance, and adjuvant chemotherapy for stage I disease.
Radiation Doses and Fields
With respect to radiation dose and schedule, the authors do an excellent job of summarizing the many single- and multi-institution studies that have been performed. Particularly pertinent are the side effects associated with radiation therapy, which can potentially be avoided by minimizing field size and decreasing radiation doses. Problems associated with infertility, cardiovascular toxicity, gastrointestinal toxicity (including peptic ulcer disease), and second malignancies (including solid tumors and leukemia) are all seen with much higher frequency in patients who receive radiation therapy.
These problems have led investigators to evaluate lower doses of radiation therapy and decreased field size. The obvious benefits of this strategy are a decrease in the extent of irradiation of bone marrow, a favorable impact on spermatogenesis, and, perhaps, a decrease in the risk of secondary tumors. Obviously, however, there is a minimal threshold of radiation that is necessary to achieve tumoricidal effects. Clinical trials evaluating radiation fields and doses, which are currently underway in Europe, are to be commended.
Pros and Cons of Surveillance
As mentioned above, with chemotherapy functioning as a successful safety net for patients with early-stage germ cell tumors, surveillance would appear to have a potential role in the management of clinical stage I seminoma. As the authors discuss, cumulative data suggest that patients who are managed with observation rather than primary radiotherapy have about a 17% risk of developing a recurrence and a long-term survival rate of approximately 97%.
These data can be looked at in two different ways. First, only 3 out of 100 patients with clinical stage I disease would be expected to die from the disease. However, for patients who develop a recurrence, the chances of dying are approximately 18% (3 ÷ 17%). Although infrequent, some patients may develop recurrent disease that is more advanced and, as a consequence, less likely to be cured by chemotherapy. The potential disadvantage of surveillance for seminomas is that, unlike nonseminomatous germ cell tumors, serum markers are not reliably elevated. Thus, there is a need for greater dependence on noninvasive radiographic studies, such as CT scans, for screening.
A potential benefit of surveillance is that only those patients who are destined to develop a recurrence receive radiation therapy. Thus, one can spare patients who do not need therapy additional long-term morbidity. It should be emphasized that the best results of surveillance have been achieved in patients who are quite meticulous about complying with follow-up evaluations. Surveillance is not meant to be a substitute for radiation therapy in patients who are not willing or able to undergo routine follow-up CT scans.
Role of Adjuvant Chemotherapy
The final issue in early-stage seminoma is the role of adjuvant chemotherapy in clinical stage I disease. Potential advantages of chemotherapy are that it avoids the potential long-term side effects of radiation therapy and that it may decrease the incidence of car-cinoma in situ (although the latter advantage has been hotly debated). The therapeutic outcome of patients treated with adjuvant chemotherapy appears to be comparable to that achieved with radiation therapy or with surveillance.
Major objections to the use of single-agent carboplatin or cisplatin stem from observations made in the systemic treatment of nonseminomatous germ cell tumors (highlighted above). Does the choice of drugs, dose, and number of cycles of therapy make a difference? I believe so, as has been proven in other prospective trials conducted in large numbers of patients.
By definition, of 100 patients with clinical stage I disease treated with totally ineffective therapy, 83% will achieve long-term survival because they are true pathologic stage I patients. Thus, the denominator of treated patients who could possible be affected by therapy is only 17. A drug that is 90% effective will cure 15 out of 17 patients, an 80% effective drug will cure roughly 13.6 patients, and a 70% effective drug will cure 12 patients. Thus, the difference between 90% efficacy and 70% efficacy amounts to 3 patients (15 patients 12 patients).
Thus, one is unlikely to find a statistically significant difference between therapies unless large numbers of patients are entered into clinical trials. Nonetheless, virtually 99% to 100% of patients with clinical stage I disease should be cured, either by primary radiation therapy or salvage chemotherapy. One should be cautious in recommending "minimal therapy" for patients unless prospective, randomized trials have proved therapeutic equivalents. No such trial has been conducted to date, and until one is done, it is my strong belief that primary chemotherapy should not be considered a therapeutic option, except in very rare circumstances. When chemotherapy is used, it is logical to prescribe the drug combinations and schedules that have proven most effective in advanced disease, rather than single-agent therapy.
Summary
As we survey the therapeutic options for patients with clinical stage I seminoma, we can feel comfortable that the vast majority of patients will have a normal life expectancy. Nonetheless, as these authors have thoughtfully done, we must also be cognizant of the long-term sequelae of our therapies. The success and failure of our therapeutic approaches can no longer be measured in the time frame surrounding therapy, but rather, in the lifetime of the patient.
Articles in this issue
over 27 years ago
CD-ROM Helps Cancer Patients Ease the Painover 27 years ago
UT Southwestern and Komen Foundation Offer Breast Care Fellowshipover 27 years ago
Genetic Switch May Yield Map of Prostate Cancer Machineryover 27 years ago
Personalized Approach Increases Breast Cancer Screening RatesNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.