- ONCOLOGY Vol 16 No 3
- Volume 16
- Issue 3
Monoclonal Antibodies in Hematologic Malignancies: Research and Clinical Developments
It is amazing how, over the past 5 years, the world of clinical research in the lymphoid malignancies has been totally redirected by one molecule called rituximab (Rituxan).
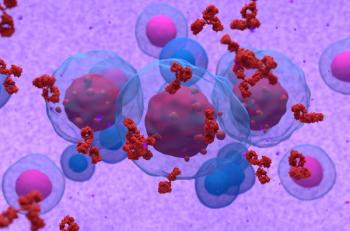
It is amazing how, over the past 5 years, the world of clinical research inthe lymphoid malignancies has been totally redirected by one molecule calledrituximab (Rituxan). Since its approval by the US Food and Drug Administrationfor the treatment of relapsed and refractory follicular and low-grade B-cellnon-Hodgkin’s lymphoma (NHL), the use of this monoclonal antibody has becomeso ubiquitous that it has earned the nickname "vitamin R." Those whoattended the 43rd Annual Meeting of the American Society of Hematology could nothelp but be overwhelmed by the number of abstracts discussing not only rituximab(more than 108), but also other new and exciting antibodies andradioimmunoconjugates, such as alemtuzumab (Campath), epratuzumab (hLL2 [LymphoCide]),yttrium-90 ibritumomab tiuxetan (Zevalin), and tositumomab/iodine-131tositumomab (Bexxar).
At no time in recent memory has so much enthusiasm been generated for newtherapies in the treatment of patients with lymphoid malignancies. These newantibodies and radioimmunoconjugates have irreversibly changed our treatmentparadigms. Clearly, it is becoming increasingly difficult to conduct a clinicaltrial in patients with NHL that either does not incorporate rituximab orexcludes patients who received prior rituximab therapy.
However, high expectations must be tempered with attention to data. We mustlearn to separate the science from the religion, the facts from the opinions (Cheson:N Engl J Med 346:280-282, 2002). Although a drug such as rituximab has afavorable toxicity profile, excessive use/abuse may lead to unexpectedcomplications from chronic B-cell depletion. Inappropriate selection of patientsfor radioimmunoconjugate therapy, such as those with greater than 25% bonemarrow involvement, decreased stem cell reserves, or a preexisting cytogeneticabnormality, may lead to profound and prolonged cytopenias or myelodysplasticsyndrome/acute myelogenous leukemia. Nevertheless, these agents offer a majoradvance over our current therapies. The possibility of moving away fromnonspecific cytotoxic therapy to less toxic targeted treatments is extremelyattractive and may hopefully lead to improved outcomes for patients withlymphoid malignancies.
We are clearly in the midst of a rapid and dramatic change in the treatmentparadigms for patients with NHL, as well as other malignant and benignhematologic disorders. The abstracts reviewed in this supplement illustrate thatclinical research in lymphoid malignancies has come a long way in a short time,but that a lot of work remains to be done.
Articles in this issue
almost 24 years ago
Single-Agent Rituximab in Early-Stage Chronic Lymphocytic Leukemiaalmost 24 years ago
Recruitment for Trial of Adjuvant Trastuzumab Under Wayalmost 24 years ago
Rituximab in the Treatment of Acquired Factor VIII Inhibitorsalmost 24 years ago
Support for New Medicare Pay Formulaalmost 24 years ago
Irinotecan-Containing Regimen Improves Survival in Small-Cell Lung CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.