Oncology NEWS International
- Oncology NEWS International Vol 8 No 9
- Volume 8
- Issue 9
MRI Can Pinpoint Invasive Lobular Breast Cancer
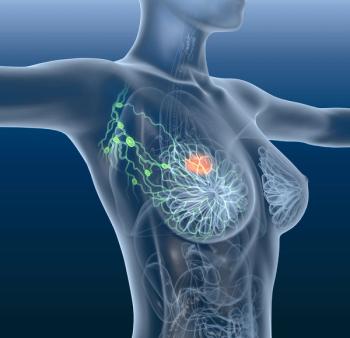
NEW ORLEANS-Magnetic resonance imaging (MRI) of the breast is more accurate than conventional methods for identifying the extent of invasive lobular carcinoma, according to a study presented at the American Roentgen Ray Society annual meeting.
NEW ORLEANSMagnetic resonance imaging (MRI) of the breast is more accurate than conventional methods for identifying the extent of invasive lobular carcinoma, according to a study presented at the American Roentgen Ray Society annual meeting.
Lobular carcinoma is difficult to detect by mammography because the tumor cells form a linear array that does not cause architectural distortion, said Rose E. Heller, MD, a fellow in the Department of Radiology, Hospital of the University of Pennsylvania, Philadelphia.
This form of cancer may be hidden within the normal breast tissue on the mammogram and therefore cannot be easily seen, Dr. Heller said. These tumors account for about 10% of breast cancers and are often multifocal in nature. Residual disease is more frequently a problem with lobular carcinoma than with infiltrating ductal carcinoma.
Dr. Heller and her colleagues studied 31 women with lobular carcinoma, 32 to 69 years old, who were enrolled in various protocols at their institution: 10 were studied following excisional biopsy, 9 had a positive screening mammogram, 8 had palpable abnormalities, 1 had a positive axillary lymph node, and 3 were excluded due to lack of clinical follow-up. Contrast-enhanced MR images were compared with mammography and ultrasound results, and correlated with pathologic findings after excision or mastectomy.
Tumor extent on MR imaging correlated with pathologic tumor extent in 89% of the cases, Dr. Heller said. In two cases, MR imaging overestimated disease extent, and, in one instance, disease extent was underestimated.
MR imaging alone accurately detected tumor extent in 20 of the 28 cases (71%), whereas in only one case was tumor extent determined accurately by mammography alone. Both MRI and mammography identified tumor extent in 5 cases.
Only 12 women had ultrasound studies performed, but in 8 cases, ultrasound underestimated tumor extent. In 4 cases, both MR imaging and ultrasound were able to accurately assess tumor extent.
Clinically, MR imaging upstaged 20 of the 28 patients. While 6 women went directly to mastectomy, 13 opted for wider excision, with 8 of them ultimately undergoing mastectomy. For 4 patients, MR imaging would have predicted the need for mastectomy initially. Thus, this procedure could be used to guide surgical planning.
Both Dr. Heller and one of her collaborators, Susan Orel, MD, commented that MR imaging could be used to plan the fastest and most accurate treatments for women with lobular breast cancer. Although our work needs to be expanded, the results are compelling for this small group, Dr. Heller said.
Articles in this issue
over 26 years ago
‘Gonzalez Diet’ to Be Tested in Pancreatic Cancerover 26 years ago
Talking to Members of Congress About Cancer Issuesover 26 years ago
Modified SPECT Scintimammography Proves More Accurateover 26 years ago
Lilly Enjoined From Promoting Evista for Breast Cancer Preventionover 26 years ago
Experts Brief Capitol Hill on Trial Costs Surveyover 26 years ago
NIH Plan Quadruples Prostate Cancer Research Fundsover 26 years ago
Gabapentin as Adjuvant to Opioids in Neuropathic Painover 26 years ago
Biochemotherapy May Be an Option in Metastatic Melanomaover 26 years ago
PET Scans Spare Some NSCLC Patients From Mediastinoscopyover 26 years ago
Computer Technique Gives New Life to Thermal Breast ImagingNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.