- ONCOLOGY Vol 13 No 7
- Volume 13
- Issue 7
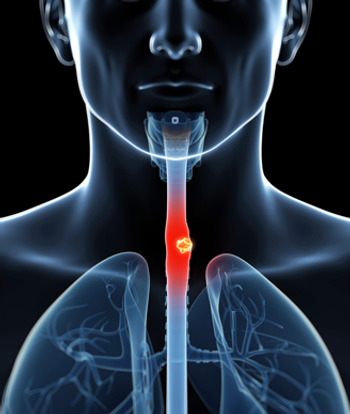
Photodynamic Therapy Effective for Swallowing Problems
Photodynamic therapy (PDT) relieves swallowing problems associated with esophageal cancer in the majority of patients treated, according to a study conducted from November 1996 to June 1998 at the University of Pittsburgh Cancer Institute.
Photodynamic therapy (PDT) relieves swallowing problems associated with esophageal cancer in the majority of patients treated, according to a study conducted from November 1996 to June 1998 at the University of Pittsburgh Cancer Institute. The study, which was presented at the 1999 meeting of the Society of American Gastrointestinal Endoscopic Surgeons in San Antonio, involved 77 patients with either primary esophageal cancer or a recurrence of disease after other treatments failed. All patients were treated with PDT.
Although further studies will need to be done in this area, we found PDT to be effective in our patients, said James D. Luketich, MD, senior coauthor of the study and assistant professor of surgery at the University of Pittsburgh. This is one of the first reports, after FDA approval of PDT, that shows that it is effective in relieving swallowing problems in patients with esophageal cancer, he said. Ninh T. Nguyen, MD, currently of the University of California at Davis and formerly with the University of Pittsburgh Medical Center, coauthored the study.
How PDT Works
During PDT, surgeons administer an injection of porfimer sodium (Photofrin). The drug remains dormant until it is activated by a nonthermal red laser light positioned at the end of a thin, fiberoptic probe. The doctor inserts this line into the patients esophagus and targets the cancer cells. Once in place, the laser light activates the drug, destroying the cancer cells and leaving the surrounding healthy tissue largely unharmed.
For the study, doctors administered 1.5 to 2 mg/kg of porfimer sodium intravenously, followed 48 hours later by the laser light treatment. Endoscopy was performed 2 days after the initial treatment to assess tumor response and debridement and to determine whether a second light treatment would be necessary. The study measured the degree of palliation by the dysphagia-free interval and through the use of a dysphagia score of 1 to 5 (where 1 represents no dysphagia and 5, complete obstruction).
All of the patients were treated with 125 courses of PDT, of which 87 were for obstruction, 6 for bleeding, and 32 for tumor ingrowth or overgrowth (the result of previously placed esophageal stents).
Dysphagia Scores Decline
Dysphagia scores improved in 90% of the patients following 4 weeks of PDT. The mean dysphagia score decreased from 3.2 preoperatively to 1.9 postoperatively, and PDT adequately controlled bleeding in the six patients treated. The mean dysphagia-free interval was 75 days, with a median survival time of 5 months. A second course of PDT was required in 38% of the patients, and an expandable metal stent was placed in 29% when tumor progression resulted in extrinsic compression.
According to Dr. Luketich, expandable metal stents typically have been used in patients with esophageal cancer and continue to play an important role in some patients. However, in some cases, stents may have significant disadvantages. These include tumor ingrowth and stent migration. Also, in some patients, severe esophageal reflux disease and pain can limit the effectiveness of the expandable metal stent.
For more information on the use of PDT as a treatment for lung or esophageal cancer, contact the University of Pittsburgh Cancer Institutes Cancer Information and Referral Service at either 1-800-237-4PCI (4724) or (412) 624-1115 or visit the institutes web site at
Articles in this issue
over 26 years ago
Discussing Disease Progression and End-of-Life Decisionsover 26 years ago
New Genetic Mechanism Associated With Thyroid-Related Diseasesover 26 years ago
Beyond 5-Fluorouracilover 26 years ago
Nonsurgical Therapy Holds Promise for Basal Cell Carcinomaover 26 years ago
Novel Gene Therapy to Clear Blood Clots in Leg Arteriesover 26 years ago
Bills Would Require Private Insurers to Pay for Cancer ScreeningNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.