
Thomas G. Martin, MD, Discusses Approval of Cilta-Cel in R/R Multiple Myeloma
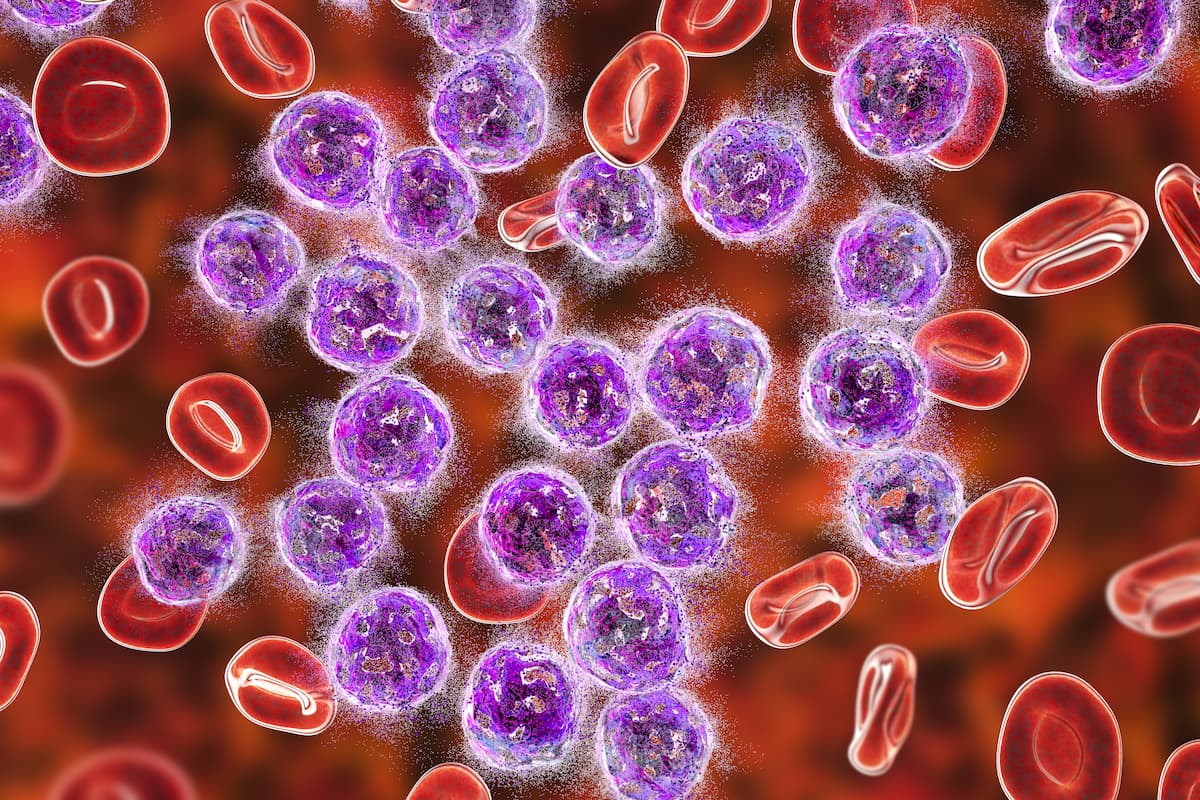
In an interview with CancerNetwork®, Thomas G. Martin spoke about how the approval of ciltacabtagene autoleucel will likely dramatically impact the standard of care for patients with relapsed/refractory multiple myeloma.
The approval comes as a results of the
“We couldn’t be more excited about cilta-cel with the current data showing that 60.5% of patients remain in remission 24 months after initiation of therapy. We can’t wait to see what it is at 30 months, and maybe what it is at 36 months. All CAR T-cell therapeutics aim to have a flattening of the curve. Unfortunately, [for] patients who have the worst myeloma are the most resistant [and] relapse over time, there might be a tail end the curve or flattening of the curve. [These are] people who have prolonged remission duration, and some may be cured. We still don’t know from the cilta-cel PFS curve if there’s going to be a tail or if there are going to be some patients who have long remission durations for 5-plus years. If that’s true, that’s amazing,” Martin stated.
In an interview with CancerNetwork®, Martin, lead study investigator of CARTITUDE-1 and associate director of the myeloma program at the University of California San Francisco, discussed the importance of the approval, how it may address unmet patient needs, and future research directions.
CancerNetwork®: What does the approval of cilta-cel in the treatment of recurrent or metastatic cervical cancer mean for this patient population?
Martin: We have quite a few patients, over 50,000, who are in the US right now who currently have multiple myeloma. A large number of those [patients are] triple-class refractory. [Sometimes patients] have very few options left for good therapeutics that provided deep remission. We have 1 CAR T-cell product that’s currently approved for use, known as idecabtagene vicleucel [Abecma]. It has been very difficult to obtain manufacturing slots, or to obtain the therapy for people across the US, so the [approval of cilta-cel] is huge. There’s room for 2, 3, maybe even 4 different CAR T-cell therapeutics based on the number of slots that we need and the number of patients who currently will be eligible for this therapy.
In this in this triple-class refractory population, we do have some drugs that are available. For the drugs that are currently available, the response rates are in the order of 20% to 30%, so only 1 in 4, or maybe 1 in 3, [patients] will respond. When they respond, they tend to respond for anywhere between 5 and 11 months; they have a short time of response, unfortunately. We’re left to recycle some of the drugs that we had before, and sometimes we don’t have medicines that’ll work. That is an unmet need for patients who’ve received our 3 big classes of drugs. [They are] proteasome inhibitors, immunomodulatory drugs, and CD38 antibodies. When they received those [drugs] and [they] don’t work anymore, we need more therapies for those patients.
Which patients will benefit most from this therapy?
We try to look at what the difference between eligibility for an autologous transplant, eligibility for a CAR T-cell therapy, or [eligibility] for any off-the-shelf product. For most people who are older than age 70, or older than age 75 years, we have a difficult time [conducting] an autologous transplant because it’s a tough treatment.
CAR T-cells can be [manufactured for] patients who are 8 years old and patients who are in their mid 80s if that patient is fit. I [ask patients] ‘if you walk [the distance of] 2 telephone poles, do you need oxygen? If you don’t, do you get chest pain?’ If you don’t, you’re eligible for CAR T-cell therapy. We can make it so that a larger population than [those] who are eligible for an autologous transplant can get this CAR T-cell therapy. Anybody who is fit, age independent, [who can] walk into the doctor’s office, jump in the chair, jump up on doctors table, etc., is likely fit enough to go through CAR T-cell therapy. It’s going to be a broad patient population. That’s why the need is so high [for this treatment].
What are the next steps for researching this product in this patient population?
In this patient population, we must look into how we can make it a longer remission duration for everybody. The currently approved therapeutic idecabtagene vicleucel has a [median] progression-free survival [PFS] of 12 months. We would love for it to be longer than that, right? Maybe we need to do maintenance therapy. Maybe we need to see if we [give] treatment after we give the CAR T-cell therapy, something that can rev up the T-cells, make them last longer, and perhaps provide more of an anti-myeloma effect.
Cilta-cel has a longer PFS [according to data recently] presented at the recent [63rd Annual American Society of Hematology Annual Meeting]. The 2-year PFS rate was 60.5%, so people are getting 2 years or more of remission duration. Can we even make it longer by adding [another agent]? That’s one avenue as to how to make it better for the people with relapsed, triple-class refractory [disease]. The other question for us is if we move it to earlier lines of therapy, will we be able to cure some patients with multiple myeloma? Will their remission duration be longer? If we do it in less heavily pretreated patients where their T-cells are healthier and when their myeloma isn’t as resistant, can we make it last longer? That’s a huge question, and that’s where a lot of the energy is now in proving those points.
References
- U.S. FDA Approves CARVYKTI (ciltacabtagene autoleucel), Janssen's first cell therapy, a BCMA-directed CAR-T immunotherapy for the treatment of patients with relapsed or refractory multiple myeloma. News release. Janssen. February 28, 2022. Accessed February 28, 2022. https://prn.to/3vskiZu
- Martin T, Usmani S, Berdeja J, et al. Updated results from CARTITUDE-1: Phase 1b/2 study of ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T cell therapy, in patients with relapsed/refractory multiple myeloma. Blood. 2021;138(suppl 1):549. doi:10.1182/blood-2021-146060
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.



































