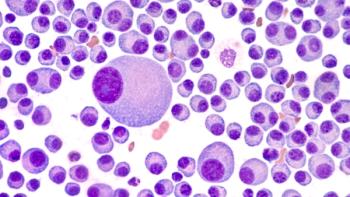
Luciano Costa, MD, PhD, spoke about the primary end point analysis for the MASTER trial examining daratumumab, carfilzomib, lenalidomide, and dexamethasone in multiple myeloma.

Your AI-Trained Oncology Knowledge Connection!

Luciano Costa, MD, PhD, spoke about the primary end point analysis for the MASTER trial examining daratumumab, carfilzomib, lenalidomide, and dexamethasone in multiple myeloma.
Daratumumab plus lenalidomide, bortezomib, and dexamethasone followed by transplant continues to show superior efficacy vs triplet therapy alone at a 2-year follow-up to the GRIFFIN trial.
A post hoc analysis showed that a dose reduction of selinexor yielded higher safety and efficacy for patients with multiple myeloma.
Patients with newly diagnosed, transplant-eligible multiple myeloma continue to experience robust and durable responses to treatment with daratumumab, lenalidomide, bortezomib, and dexamethasone plus autologous stem cell transplant followed by daratumumab plus lenalidomide maintenance.
In an assessment of 2 patient cases of relapsed or refractory multiple myeloma with translocations in t(11;14), selinexor plus venetoclax was safe and efficacious.

The treatment combination of selinexor plus pomalidomide and dexamethasone at the recommended phase 2 dose produced more durable and deep responses than the lesser selinexor dose for relapsed or refractory multiple myeloma.

Induction and consolidation with daratumumab, ixazomib, lenalidomide, and dexamethasone was able to induce minimal residual disease in a subset of patients with transplant-eligible newly diagnosed multiple myeloma and standard-risk disease.
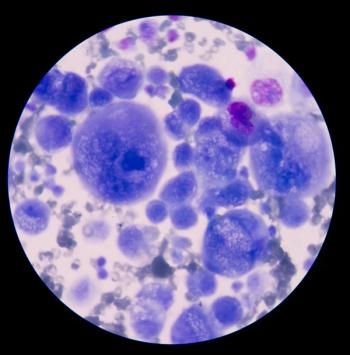
Among patients with newly diagnosed multiple myeloma, 80% of a study cohort reached MRD negativity following treatment with daratumumab, carfilzomib, lenalidomide, and dexamethasone.
Weekly selinexor combined with bortezomib and dexamethasone appears to be a promising option in patients with high-risk multiple myeloma.

A population of patients with relapsed/refractory multiple myeloma appeared to benefit from treatment with selinexor plus daratumumab, bortezomib, and dexamethasone
Adding isatuximab to lenalidomide, bortezomib, and dexamethasone demonstrated a superior minimal residual disease rate in patients with transplant-eligible newly diagnosed multiple myeloma.
The combination of daratumumab with bortezomib, cyclophosphamide, and dexamethasone continued to improve hematologic and organ responses after 18 months of follow-up.
Findings from the phase 1b TRIMM-2 study indicated that patients with relapsed/refractory multiple myeloma experienced manageable toxicities and promising responses to treatment with talquetamab and daratumumab.
Research presented at the 63rd ASH Annual Meeting and Exposition found significantly higher MRD-negativity and sustained MRD-negativity rates among patients with transplant-eligible newly diagnosed multiple myeloma receiving D-VTd over VTd alone.
Patients with newly diagnosed multiple myeloma who are non-transplant eligible and intermediate-fit and who received a less toxic regimen of ixazomib, daratumumab, and low-dose dexamethasone demonstrated higher rates of objective response.

A phase 2 trial shows promise of the daratumumab/ixazomib combination in frail and elderly patients with multiple myeloma who are treated in the relapsed setting when given without dexamethasone.
Patients receiving daratumumab, lenalidomide, and dexamethasone in the first line saw better overall survival than those who waited and received second-line daratumumab-based regimens for transplant-ineligible newly diagnosed multiple myeloma.
Thomas G. Martin, MD, spoke about different abstracts to be presented at ASH 2021.

The expert in multiple myeloma highlighted the research which she was most excited to see presented at the ASH Annual Meeting & Exposition.
Hypogammaglobulinemia was found to be nearly universal for patients with multiple myeloma during treatment with daratumumab, suggesting a role for intravenous immunoglobulin.

The director of clinical research in the Center for Cancer Care at White Plains Hospital spoke about what she intends to evaluate for a patient population with multiple myeloma and diabetes moving forward.
Jeffrey Wolf, MD, explained how studies presented at the recent 2020 ASH Annual Meeting & Exposition did not report what percentage of patients achieved minimal residual disease negativity with therapy for multiple myeloma, and that the future of phase 3 trials should focus on this status in patients.
The ongoing phase 1/2 DREAMM-6 trial found that the addition of belantamab mafodotin to bortezomib and dexamethasone elicited high response rates and a suitable safety profile in patients with relapsed or refractory multiple myeloma.
Daratumumab plus lenalidomide, bortezomib, and dexamethasone improved response rates and depth of response in patients with transplant-eligible, newly diagnosed multiple myeloma.

TNB-383B was well tolerated and researchers saw significant responses when it was administered at a higher dose level for heavily pretreated patients with relapsed/refractory multiple myeloma.
Data presented at the 2020 ASH Meeting found talquetamab elicited a high response rate with a tolerable safety profile for patients with relapsed/refractory multiple myeloma.
The myeloma expert discussed the randomized, open label study measuring the safety and efficacy of daratumumab (Darzalex) plus RVd for patients with newly diagnosed multiple myeloma.
Cevostamab, a FcRH5xCD3 bispecific antibody, was safe and highly active when treating heavily pretreated patients with relapsed/refractory multiple myeloma, according to data presented at the 2020 ASH Annual Meeting & Exposition.

The BCMA- and CD3-targeted bispecific monoclonal antibody, demonstrated early, deep, and durable responses with acceptable safety and tolerability in patients with relapsed/refractory multiple myeloma.

The combination induced low rates of infusion-related reaction, and had a shorter administration duration, increasing convenience for patients and decreasing treatment burden, according to Meletios A. Dimopoulos, MD.