
Real-world data show that CAR T-cell therapy may be considered for eligible patients with relapsed/refractory multiple myeloma harboring CNS involvement.

Your AI-Trained Oncology Knowledge Connection!


Real-world data show that CAR T-cell therapy may be considered for eligible patients with relapsed/refractory multiple myeloma harboring CNS involvement.

Lisaftoclax with pomalidomide and dexamethasone elicited positive efficacy and safety outcomes in relapsed/refractory multiple myeloma.
In patients with lens-refractory multiple myeloma, cilta-cel generated deeper minimal residual disease rates across all patient subgroups.
Pelabresib and ruxolitinib combination maintains consistent reduction of symptoms and anemia in patients with myelofibrosis.
Patients with newly diagnosed multiple myeloma experienced sustained MRD negativity with isatuximab/bortezomib/lenalidomide/dexamethasone.

Findings from DREAMM-7 support belantamab mafodotin plus bortezomib and dexamethasone as a standard of care in relapsed/refractory multiple myeloma.

Using bispecific antibodies before or after CAR T-cell therapy in multiple myeloma is an area of education for community oncologists.
All evaluable patients achieved minimal residual disease negativity following teclistamab-based treatment in the phase 3 MajesTEC-4/EMN30 trial.
PFS and OS were significantly improved with subcutaneous daratumumab vs active monitoring in patients with smoldering multiple myeloma.
Daratumumab plus VRd showed a deepened MRD and PFS rate for patients with transplant-ineligible or -deferred newly diagnosed multiple myeloma.

GPRC5D may be a promising therapeutic pathway in the treatment of those with relapsed/refractory multiple myeloma, says Susan Bal, MD.
Data from the phase 1b MonumenTAL-2 trial support pomalidomide plus talquetamab as a promising treatment option in relapsed/refractory multiple myeloma, says Jeffrey Matous, MD.

Isatuximab plus carfilzomib, lenalidomide, and dexamethasone demonstrates durable responses in patients with newly diagnosed standard- and high-risk multiple myeloma.
Treatment with anito-cel produces deep, enduring responses in high-risk relapsed/refractory multiple myeloma, says Matthew Frigault, MD.

The safety profile of idecabtagene vicleucel in relapsed/refractory multiple myeloma following the first 3 months of treatment appears to be comparable with standard therapies, says Rachid Baz, MD.
Data from the phase 3 PERSEUS trial supports D-VRd followed by DR maintenance as a new standard of care in patients with newly diagnosed, transplant-eligible multiple myeloma.
The addition of isatuximab to carfilzomib/lenalidomide/dexamethasone appears to be manageable with respect to safety and tolerability in treating patients with newly diagnosed multiple myeloma, according to data from the phase 3 IsKia trial.
Early phase data found that use of D8 Fab CAR results in increased responses and activity for patients with relapsed/refractory multiple myeloma.
The assessment of health-related quality of life for patients with previously treated multiple myeloma was found to be enhanced in the phase 3 KarMMa-3 trial when patients were treated with idecabtagene vicleucel.
The use of teclistamab in the real-world phase 2 MajesTEC-1 analysis showed similar safety and efficacy for patients with relapsed/refractory multiple myeloma.

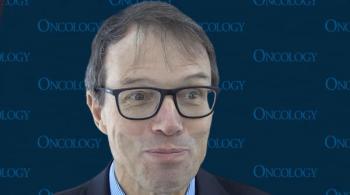
CancerNetwork® spoke with Rafael Fonseca, MD, about future efforts to compare use of daratumumab-containing regimens as either frontline or second-line therapy in patients with multiple myeloma that are transplant ineligible.

CancerNetwork® spoke with Rafael Fonseca, MD, about findings from a simulation using real-world data sets to compare the utility of daratumumab-containing regimens as either frontline or second-line therapy.
A triplet combination of belantamab mafodotin-blmf plus pomalidomide and dexamethasone yielded a manageable safety profile in a population of patients with relapsed/refractory multiple myeloma.

CancerNetwork® spoke with Rafael Fonseca, MD, about real-world use of daratumumab-containing regimens as either frontline or second-line therapy for transplant-ineligible multiple myeloma.
Luciano Costa, MD, PhD, spoke about the potential application of daratumumab, carfilzomib, lenalidomide, and dexamethasone for multiple myeloma in a real-world setting.
Prognostic awareness impacted patients quality of life through psychosocial distress and symptoms burden.

CancerNetwork® spoke with Rafael Fonseca, MD, about the rationale for a simulation using real-world data sets to compare the utility of daratumumab-containing regimens as either frontline or second-line therapy.
Luciano Costa, MD, PhD, spoke about how the results in the final primary analysis of the MASTER trial with daratumumab, carfilzomib, lenalidomide, and dexamethasone in multiple myeloma were not what he expected.
Patients with heavily pretreated relapsed/refractory multiple myeloma achieved promising benefit in terms of cytokine release syndrome mitigation via double cycle 1 step-up dosing for cevostamab.
Patients with relapsed/refractory t(11;14) multiple myeloma appeared to benefit from treatment with venetoclax at a dose of 400 mg or 800 mg plus daratumumab/dexamethasone.