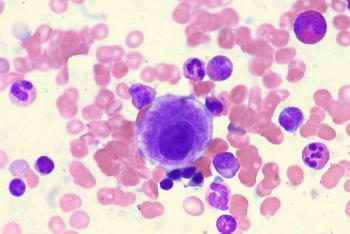
Patients with previously untreated diffuse large B-cell lymphoma experienced promising responses after being treated with tafasitamab-cxix and lenalidomide plus rituximab, cyclophosphamide, doxorubicin, vincristin, and prednisone.

Your AI-Trained Oncology Knowledge Connection!

Patients with previously untreated diffuse large B-cell lymphoma experienced promising responses after being treated with tafasitamab-cxix and lenalidomide plus rituximab, cyclophosphamide, doxorubicin, vincristin, and prednisone.

Data from a retrospective head-to-head analysis of pacritinib vs ruxolitinib showed that the former was more favorable in terms of symptom response for patients with myelofibrosis and thrombocytopenia.
The combination of high-frequency and low-dose acalabrutinib and rituximab demonstrated a 100% overall response rate in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma.

Acalabrutinib produced positive quality-adjusted survival benefits over other treatment options for patients with relapsed/refractory chronic lymphocytic leukemia.

A post-hoc analysis of a phase 3 trial presented at 2021 ASH indicate that acalabrutinib may be favorable in terms of toxic burden and cardiovascular-related events when compared against ibrutinib for treating chronic lymphocytic leukemia.
Patients with cytopenic myelofibrosis produced a tolerable safety profile when receiving treatment with pacritinib.

A phase 2 study has begun recruiting patients with relapsed/refractory acute myeloid leukemia to test the efficacy of magrolimab.
Patients with relapsed/refractory multiple myeloma continue to experience robust and durable benefit from treatment with ciltacabtagene autoleucel.
Patients with polycythemia vera who have controlled hematocrit and elevated white blood counts can have increased risk of thrombotic events.

YTB323 led to a promising safety profile and encouraging efficacy outcomes for adult patients with relapsed/refractory diffuse large B-cell lymphoma.
Patients with relapsed/refractory t(11;14) multiple myeloma appeared to benefit from treatment with venetoclax at a dose of 400 mg or 800 mg plus daratumumab/dexamethasone.
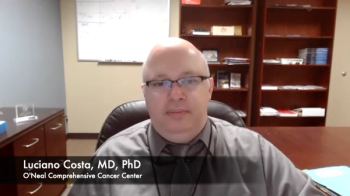
Luciano Costa, MD, PhD, spoke about the primary end point analysis for the MASTER trial examining daratumumab, carfilzomib, lenalidomide, and dexamethasone in multiple myeloma.
Patients with low-risk myelodysplastic syndrome saw more durable responses and higher tolerability when taking luspatercept-aamt compared with the placebo.
Daratumumab plus lenalidomide, bortezomib, and dexamethasone followed by transplant continues to show superior efficacy vs triplet therapy alone at a 2-year follow-up to the GRIFFIN trial.
A post hoc analysis showed that a dose reduction of selinexor yielded higher safety and efficacy for patients with multiple myeloma.

Patients with high-risk large B-cell lymphoma saw durable responses when treated with axicabtagene ciloleucel.
A 27% reduction in the risk of progression or death was noted when polatuzumab vedotin was added on R-CHP vs R-CHOP for patients with intermediate- or high-risk diffuse large B-cell lymphoma who received treatment in the first line.
Standard of care treatment was superior to the combination of ibrutinib plus venetoclax in terms of decreasing minimal residual disease for previously untreated patients with chronic lymphocytic leukemia.

Sattva S. Neelapu, MD, spoke about which abstracts he was most excited to see presented at the upcoming American Society of Hematology Annual Meeting.
The time-limited combination of ibrutinib plus chemoimmunotherapy in younger fit patients with chronic lymphocytic leukemia increased the rate of complete responses with bone marrow undetectable minimal residual disease, regardless of IGHV mutation, according to long-term follow-up data.
Patients with newly diagnosed, transplant-eligible multiple myeloma continue to experience robust and durable responses to treatment with daratumumab, lenalidomide, bortezomib, and dexamethasone plus autologous stem cell transplant followed by daratumumab plus lenalidomide maintenance.

Ciltacabtagene autoleucel as a single infusion led to early, durable responses, and demonstrated positive minimal residual disease negativity for patients with multiple myeloma who had early clinical relapse.

A positive overall response rate was achieved when patients with relapsed/refractory peripheral T-cell lymphoma were treated with duvelisib plus romidespin.
Patients with large B-cell lymphoma who were previously excluded from investigations experienced increased efficacy with the use of axicabtagene ciloleucel.
Patients with relapsed or refractory aggressive B-cell non-Hodgkin lymphoma did not benefit in terms of event-free survival when treated with the CAR T-cell therapy tisagenlecleucel vs standard-of-care chemotherapy and transplant.
In an assessment of 2 patient cases of relapsed or refractory multiple myeloma with translocations in t(11;14), selinexor plus venetoclax was safe and efficacious.
Patients with previously untreated chronic lymphocytic leukemia derived a better progression-free survival benefit from treatment with ibrutinib and rituximab vs fludarabine, cyclophosphamide, and rituximab.

Glofitamab monotherapy or in combination with obinutuzumab led to strong response rates for patients with multiple relapsed or refractory follicular lymphoma.
Elderly patients treated with ibrutinib-containing regimens for chronic lymphocytic leukemia saw a progression-free survival benefit vs those who received rituximab and bendamustine.

The treatment combination of selinexor plus pomalidomide and dexamethasone at the recommended phase 2 dose produced more durable and deep responses than the lesser selinexor dose for relapsed or refractory multiple myeloma.