
Developers plan to discuss a regulatory path to conditional marketing authorization for OST-HER2 in the UK, US, and EU in resected metastatic osteosarcoma.

Your AI-Trained Oncology Knowledge Connection!


Developers plan to discuss a regulatory path to conditional marketing authorization for OST-HER2 in the UK, US, and EU in resected metastatic osteosarcoma.
Andrzej Jakubowiak, MD, PhD, prioritizes KRd-based regimens for the treatment of high-risk newly diagnosed disease in the posttransplant setting.

A new clinical trial aims to offer a novel allogenic CAR T-cell product for patients with lymphoma closer to home.

The 10-year biochemical DFS rate was 86% with EBRT plus focal boost vs 71% with standard EBRT in those with intermediate- and high-risk prostate cancer.
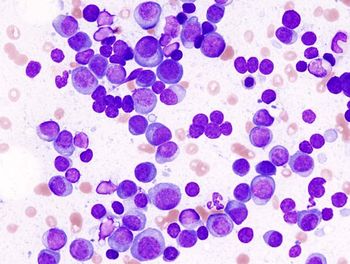
Although a similar proportion achieved MRD negativity at the 10 to the –6 power, not enough studies have analyzed MRD at this level for multiple myeloma.

Determining the molecular characteristics of one’s disease may influence the therapy employed in the first line as well as subsequent settings.
Data from a phase 1/1b trial showed that WTX-124 achieved clinically meaningful activity in those with advanced melanoma following SOC immunotherapy.

Unique toxicities presented with talquetamab tend to get progressively better as the treatment course continues, according to Prerna Mewawalla, MD.

Modification of REMS programs may help patients travel back to community practices sooner, according to Suman Kambhampati, MD.

Kelly Dyckman, MSW, LCSW, offers advice for caregivers of patients with cancer, emphasizing the need for proactive self-care and recognizing burnout.

Symposiums and regional meetings may expand knowledge of how to adopt novel CAR T-cell therapies and bispecific antibodies, said Suman Kambhampati, MD.

Findings from the phase 3 C-POST trial support the FDA approval of cemiplimab in this cutaneous squamous cell carcinoma population.

Imaging developments have made it possible to detect nodal recurrence at low PSA levels, which could help guide salvage approaches for prostate cancer.

Brachytherapy plaque with vitrectomy and silicone oil was most often given to patients with uveal melanoma tumors sized 2 mm or larger.
Data from the phase 3 DESTINY-Breast09 trial presented at the 2025 ASCO Annual Meeting formed the basis of the supplemental NDA.

Physical therapists may play a key role in patient care before, during, and after treatment for cancer, according to Alison Ankiewicz, DPT, PT.

Kelly Dyckman, MSW, LCSW, discusses the need for proactive, not reactive, communication about posttreatment challenges to better support cancer survivors.
Prophylactic steroid or tocilizumab use may help in preventing CRS in patients undergoing treatment with bispecific antibodies for multiple myeloma.
Oncotype DX 21-gene recurrence scores may help select certain patients who are suitable to omit radiotherapy for early-stage breast cancer.

Cryoablation, when combined with adjuvant endocrine therapy, may offer a minimally invasive outpatient strategy in older patients with breast cancer.

Recommending counseling sessions may help patients with cancer navigate sexual health and emotional issues during their cancer treatment.

Tara A. McCannel, MD, PhD, discusses how brachytherapy plaque with vitrectomy and silicone oil led to a 100% survival rate in patients with uveal melanoma.

Kelly Dyckman, MSW, LCSW, discusses how her role integrates with multidisciplinary oncology teams to support patients' emotional and relational well-being.
The regulatory agency gave a PDUFA target action date of April 6, 2026, for Orca-T among patients with AML, ALL, and MDS.
Patients with multiple myeloma who received palonosetron, dexamethasone, aprepitant, and olanzapine achieved a 44.1% CR rate across all study phases.

Data support the intravesical mitomycin solution’s role as an innovative option for those with recurrent, low-grade, intermediate-risk NMIBC.

The safety profile of dato-DXd was consistent with previous clinical trials assessing the agent in breast cancer.

Casdatifan, administered at 100 mg once daily, achieved a confirmed ORR of 35% in patients with pretreated metastatic kidney cancer.

Patients with uveal melanoma who have tumors larger than 2 mm are candidates for brachytherapy plaque with vitrectomy and silicone oil.
A panel of oncology pharmacists discusses the role of lifileucel in metastatic melanoma and other considerations for using cellular therapy in solid tumors.