
A phase III study showed that APF530 could improve control of emesis in cancer patients receiving highly emetogenic chemotherapy.

Your AI-Trained Oncology Knowledge Connection!


A phase III study showed that APF530 could improve control of emesis in cancer patients receiving highly emetogenic chemotherapy.

A new study found that magnetic resonance imaging (MRI) screening improved the detection of small, high-grade breast cancers in women with average risk.

Rural cancer patients often face substantial barriers to receiving optimal treatment, including availability of cancer care providers, distance to services, lack of public transportation, financial barriers, and limited access to clinical trials. However, a number of promising approaches may address some of these challenges.

Current data challenge the statement that recommendations for postmastectomy radiotherapy should be based on the highest clinical or pathologic stage. Instead, data suggest that in a majority of patients, the pathologic stage after neoadjuvant chemotherapy carries more prognostic value.

As technology has affected every segment of society, we in the oncology community have a responsibility to make every effort to utilize these advances to enable the broadest possible outreach to our patient population in a continual process of quality improvement.

A high number of patient life-years are lost to regulatory delays for drug approvals, according to an analysis presented at the 2015 World Conference on Lung Cancer.

According to a recent study, treatments aimed at preventing skeletal-related events in patients with advanced cancer and bone metastases could reduce pain and the need for opioids.
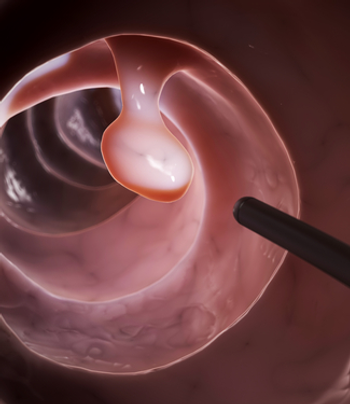
A payment system for colonoscopies offering full insurance coverage at low-priced facilities and cost sharing at high-priced alternatives reduced spending with no increase in complications.

Adding pertuzumab to first-line therapy for HER2-positive breast cancer has been shown to yield a survival benefit, but a new analysis says adding the drug is not cost effective.

The US Food and Drug Administration has approved rolapitant for the prevention of delayed phase nausea and vomiting associated with chemotherapy.

Perineural invasion was a significant predictor of increased risk for bone metastases in men with prostate cancer who had suspicion for bone metastases after a whole-body bone scan.

No matter how much education my staff and I participate in, we will never cover every single possible adverse event that an individual may experience. And in some cases, when a patient can't explain their symptoms, we can be at a loss as to how to help them.


Warfarin and a low molecular-weight heparin produced similar results in reducing major blood clots in cancer patients treated for acute venous thromboembolism.

A basket trial of patients with various nonmelanoma BRAF-mutated cancers has shown that additional tumor types may also be responsive to vemurafenib.

In my own practice, advance care planning is a part of every history and physical. In the beginning, I found the topic awkward and uncomfortable to bring up with my patients.

If we can successfully initiate advance care planning discussions with our patients and families, their end-of-life processes will improve, resulting in better care, less use of the hospital, and more honoring of newly discerned choices.

During my first medical school clinical rotation 40 years ago, the professor asked: “What’s the most important tool needed to take care of a patient?” His answer: a chair.
In the long term, ICD-10 has the potential to benefit oncology through improved data collection, but right now, practices just need to focus on preparing for the change. Here are 10 tips for oncologists.

The high cost of new cancer treatments is both ridiculous and unsustainable, but be careful when fighting “greed” by calls for regulation and price controls.

While the risk of a new treatment-related cancer diagnosis after childhood is known, a new study now shows that this risk remains into the fifth and sixth decade of life.

Hypofractionated radiation therapy results in less toxicity and provides a better quality of life compared with conventional whole-breast irradiation, according to two recent studies.

By exploring gene expression variables in addition to clinicopathologic variables, researchers were able to better predict which melanoma patients would have sentinel lymph node biopsy positivity.

This article will describe the historic background of Ra-223; outline the clinical studies which led to phase III trials of this agent; highlight key results of these phase III studies; and explore possible future directions for use of Ra-223 and other alpha particles-both in prostate cancer and for management of other diseases.

Elucidation of the underlying mechanisms of action for Ra-223 will soon expand its clinical utility with respect to improved patient selection and integrated bone-targeted therapies.

The use of CT-guided radiofrequency ablation is well tolerated and effective among patients with inoperable stage IA non-small-cell lung cancer.

Occult maternal malignancies can be detected through noninvasive prenatal testing (NIPT), according to the results of a small preliminary study.

Cancer survivors may face discrimination by adoption agencies, many of which require medical histories and statements of health to be shared with birth mothers.

How do you know your patients are cancer-free? Often hard to answer and often asked with a note of fear suggesting they don't really want to know the answer.

While having an advance plan for end-of-life decisions has increased in cancer patients, aggressive treatments near the end of life continue to occur.