
With the goal of helping to standardize and optimize care, ASCO has issued two new clinical guidelines on treating patients with HER2-positive breast cancer.

Your AI-Trained Oncology Knowledge Connection!


With the goal of helping to standardize and optimize care, ASCO has issued two new clinical guidelines on treating patients with HER2-positive breast cancer.

Oncologists are always queried about how to “eat better so my cancer doesn’t come back.” I have found the most common food issue to be the role of soy in the diet, particularly for hormone-driven breast and prostate cancer patients.

Cancer patients who are of reproductive age (especially women) can be a challenge to treat when it comes to fertility, birth control during treatment, and treatment administration during pregnancy. And for women diagnosed with cancer during pregnancy, safe treatment options need to be considered.

With the boom of technological advances and the increased use of social media come the potential ethical issues surrounding patient privacy and confidentiality.
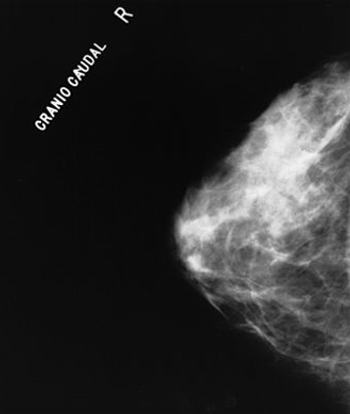
Physicians can help older women make informed mammography decisions by taking into account life expectancy and the harms and benefits of breast cancer screening.

This appendix highlights selected websites that are developed especially for oncology professionals, researchers, and patients with cancer.

ASCO has released guidelines for the prevention and management of symptoms such as anxiety, depression, fatigue, and neuropathies, which affect many cancer survivors.

Results from two large cohorts indicated that increasing blood pressure levels were associated with an increased risk for developing kidney cancer among both men and women.

The FDA has approved an HPV DNA test to be used as a primary screening method for cervical cancer in women 25 and older. The test can also give insight into future risk of cervical cancer.
Although e-cigarettes are being put forward as a safer alternative that delivers nicotine without carcinogens and assists smokers to quit, I remained concerned that evidence suggests the products are marketed for purchase and use by children. How else can one explain brands featuring flavors like Gooey Butter Cake, Snicker Doodle, Extra Sweet Cotton Candy, Bananalicious, and-the most outrageous-Gummi Bear.

This slide show features some of the highlights from the 105th Annual Meeting of the American Association for Cancer Research (AACR).

This slide show includes highlights from the 2014 Society of Gynecologic Oncology annual meeting, including one study showing bariatric surgery could lower the risk of uterine cancer, and another that found a PARP inhibitor active in BRCA-positive ovarian cancer.

Men who used sildenafil (Viagra) had an 84% increased risk for developing melanoma, even after adjusting for known risk factors, according to the results of a prospective study.

There is no question that radiopharmaceuticals have a role in the management of patients with metastatic bone disease. There is also no question that fractionated external beam radiotherapy (EBRT) is highly effective and generally well tolerated when delivered with large open or focal fields.

In order to achieve maximum survival of patients with metastatic castration-resistant prostate cancer, the judicious use of all available effective agents and modalities is required. Both EBRT and radium-223 are effective at relieving pain, but both may decrease bone marrow function.

As new data and new treatment options emerge, palliative radiotherapy algorithms will need to undergo continuous modifications and updates to ensure that patients receive optimal symptom relief.

Moving forward, perhaps no recent development in the use of RT in metastatic prostate cancer has captured greater attention than the use of radium-223 in metastatic castration-resistant prostate cancer (mCRPC).

This review will include discussion of the role of radiation therapy for osseous metastases and metastatic spinal cord compression, as well as the use of radiopharmaceuticals for painful osseous metastases.

It is important for all of us now and then to take a step back and recapture the wonder that we all felt at the onset of our careers, when treatments we now consider simple and routine held an aura of miracle. For me, a little bit of that wonder returns every time I treat a patient with a bony metastasis-in particular, from prostate cancer.

I find it difficult to put a price tag on what I do. It is mainly a thinking profession we are in, though in recent years it has become more like data entry!

Multidisciplinary care teams are an important aspect of patient-centered care and are slowly become more common place at community cancer centers. For those working at smaller hospitals or centers, it is important to use every type of resource available and in a lot of cases those resources include the nonclinical care force including family members, clergy, and volunteers.

By the year 2020 it is estimated that about 18% of the US population will be Medicare eligible and growing advances in the treatment of cancer have significantly increased the number of cancer survivors. These two growing populations have large implications on the demand for cancer services.

A session at the ACCC annual meeting addressed some of the top reimbursement issues associated with clinical trials and some strategies for how to manage them.

At the ACCC annual meeting, Jessica Turgon, MBA, from ECG Management Consultants discusses how and why providers and payers are beginning to work together to explore alternate payment models in oncology.

In 2011, the American College of Surgeons Commission on Cancer announced several new patient-centered standards that were designed to ensure that key elements of quality cancer care are provided to every person with cancer treated at an accredited facility.

An FDA panel has recommended that a DNA test that screens for HPV in women can replace the standard Pap smear as a first-line primary cervical cancer screening test.

The Society of Gynecologic Oncology (SGO) recently issued two new clinical practice statements recommending genetic testing for all women with endometrial and ovarian cancers, regardless of family history.

New guidelines supporting the broader use of sentinel lymph node biopsy in women with early-stage breast cancer have been issued by ASCO.

In this interview we preview the 2014 annual meeting of the Association of Community Cancer Centers with Matthew Farber, director of provider economics and public policy for the association.

In order to remain independent, community oncologists must align themselves with a critical mass of providers in their local or regional markets and be prepared to accept more financial risk for the quality and cost of care they provide.