Oncology NEWS International
- Oncology NEWS International Vol 19 No 7
- Volume 19
- Issue 7
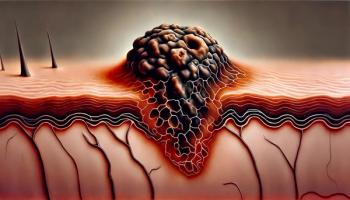
BRAF inhibition may enhance immunotherapy in melanoma
A preclinical study provides the rationale for combining BRAF-targeted therapy with immunotherapy agents in patients with BRAF mutations. These mutations activate the MAPK signaling pathway, which leads to increased oncogenic potential. The researchers showed that in BRAF-mutant melanoma cell lines, a selective BRAF inhibitor (PLX4720) blocked the MAPK pathway and increased tumor antigen expression without affecting T-cell function.
A preclinical study provides the rationale for combining BRAF-targeted therapy with immunotherapy agents in patients with BRAF mutations. These mutations activate the MAPK signaling pathway, which leads to increased oncogenic potential. The researchers showed that in BRAF-mutant melanoma cell lines, a selective BRAF inhibitor (PLX4720) blocked the MAPK pathway and increased tumor antigen expression without affecting T-cell function.
The research builds on previous clinical studies of melanoma treated with selective BRAF and MAPK inhibitors (see
"If you treat with a MAPK inhibitor, your T-cell function is decreased; your immune system is essentially repressed." - JENNIFER A. WARGO, MD
In the study, tumor antigenic expression was increased in the melanoma cell lines treated with the BRAF inhibitor (BRAF mutant lines only) or two specific MAPK/MEK inhibitors. This included an increase in melanocyte differentiation antigens (MDAs), which led to improved recognition by MART-1-specific and gp100-specific T cells.
"If indeed these BRAF inhibitors are not only killing tumor cells directly but also making the tumor cells more visible to the immune system, then treating with BRAF inhibitors may be advantageous when used in combination with immunotherapy for melanoma," Dr. Wargo said.
Expression of MDAs was proportionally upregulated in each cell line; however, the level of induction or change varied significantly, from twofold induction in one cell line to 100-fold induction in another. In future clinical trials, this variability in MDA expression changes with BRAF inhibition may help identify those patients most likely to benefit from the addition of immunotherapy.
TABLE BRAF and MAPK BRAF = B-Raf proto-oncogene serine/threonine-protein kinase
MAPK = mitogen-activated protein kinase
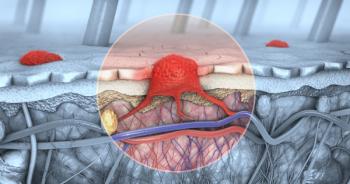
Unlike the two specific MAPK/MEK inhibitors, which decreased T-cell function, selective inhibition of BRAF had no deleterious effect on T cells. "Essentially, you could treat patients with this BRAF inhibitor and give them immunotherapy and you wouldn't be thwarting your efforts. Whereas if you treat with a MAPK inhibitor, your T-cell function is decreased; your immune system is essentially repressed," Dr. Wargo said. "I think the study has immediate clinical implications."
The study offers new arguments for combining selective targeted therapy with immunotherapy, according to Mario Colombo, PhD, senior editor for Cancer Research and director of molecular immunotherapy at the Italian National Cancer Institute in Genoa. It also offers support for further research into vaccination as a cure and prevention for melanoma, Dr. Colombo said.
Articles in this issue
over 15 years ago
Cheson heads Lymphoma Research Foundation boardover 15 years ago
SGO survey offers snapshot of gynecologic oncologyover 15 years ago
Who's Newsover 15 years ago
Earthworms: Harnessing one of nature’s cancer killersover 15 years ago
Minorities benefit from more sophisticated colon cancer screeningover 15 years ago
Imaging leader scolds payers for shortchanging cancer patientsover 15 years ago
Some ovarian tumors can be safely followed on ultrasoundNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.