- ONCOLOGY Vol 13 No 12
- Volume 13
- Issue 12
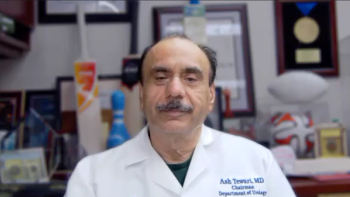
Commentary (Kavoussi)-Testicular Cancer: What’s New in Staging, Prognosis, and Therapy
Experienced authors Richard Foster and Craig Nichols providea thoughtful, state-of-the-art discussion of current controversies in the management of testicular cancer. Present cure rates illustrate that significant diagnostic, chemotherapeutic, and surgical advances made over the past century have transformed testicular cancer from a once uniformly fatal disease into a tremendous oncologic success story.
Experienced authors Richard Foster and Craig Nichols providea thoughtful, state-of-the-art discussion of current controversies in the management of testicular cancer. Present cure rates illustrate that significant diagnostic, chemotherapeutic, and surgical advances made over the past century have transformed testicular cancer from a once uniformly fatal disease into a tremendous oncologic success story. As such, secondary issues (eg, morbidity, patient anxiety, and economic considerations) have become primary concerns that must be addressed in the 21st century. Our dual charge is to pursue therapeutic methods that further increase cure rates while decreasing the morbidity associated with treatment.
Over the past decade, research efforts have focused on developing minimally invasive approaches to treat these diseases. This focus has been fueled by patient desires and new technologic developments in video and instrumentation design.
When compared to traditional open surgery, laparoscopic approaches result in less postoperative pain, quicker convalescence, and an optimal cosmetic result. Indeed, laparoscopic procedures (eg, cholecystectomy, Nissan fundoplication, adrenalectomy, nephrectomy, and oophorectomy) have become the preferred method or an acceptable alternative for treating many diseases that require surgical intervention.
The fundamental difference between a laparoscopic approach and traditional open surgery is the route of accessing pathology. The goals of surgery and actual internal manipulation are equivalent, and experienced laparoscopic surgeons can perform procedures requiring very delicate dissection and reconstruction (eg, donor nephrectomy and pyeloplasty).[1,2]
Laparoscopic vs Open Retroperitoneal Lymphadenectomy
In an effort to decrease the morbidity associated with the significant incision required with open retroperitoneal lymph node dissection in patients with testicular cancer, several centers have applied laparoscopic surgical techniques in this setting.[3-6] These techniques evolved from experience gained using pelvic lymphadenectomy to stage prostate cancer, which demonstrated that laparoscopy is equivalent to open dissection.[7] Laparoscopic retroperitoneal lymphadenectomy also has been shown to be an effective staging tool in patients with select gynecologic malignancies.[8]
Initial experience with laparoscopic retroperitoneal lymph node dissection in patients with testicular cancer demonstrated that a complete dissection can be performed without the need for a large incision. The amount and location of nodal tissue removed with a laparoscopic procedure are equivalent to those reported with open surgery.[3] Accurate pathologic staging can be achieved with less pain, rapid convalescence, and an optimal cosmetic result.
The authors cite evidence that cure rates for patients with low-stage disease may be equivalent regardless of initial management, and, thus, there may be no need for initial accurate pathologic staging when treating patients with testes cancer. However, I would argue that there is an important role for the early identification of individual patients who will later develop metastatic disease.
All of the current therapeutic options have well-recognized shortcomings, and many patients are not appropriate candidates for primary surveillance. Only through accurate staging can the most effective management scheme be crafted for each individual patient. A focused treatment plan is pivotal to minimizing morbidity, decreasing anxiety, allowing for the most cost-effective approach, and permitting patients to rapidly return to a “normal” life. Further research evaluating histologic, genetic, biological, and radiographic features may hold clues for determining which patients will ultimately develop recurrent retroperitoneal or distant disease.
Role of Adjuvant Chemotherapy in Pathologic Stage II Disease
My philosophy regarding the role of chemotherapy in patients with pathologic stage II disease detected during lymphadenectomy differs from that of Foster and Nichols. The authors have previously published their experience with open retroperitoneal lymph node dissection, which demonstrated no recurrences in their operative template.[9] As such, limited sampling has been condemned because of the risk of chemoresistant retroperitoneal recurrences. However, in a subset of patients in whom tumor recurred outside of the operative field, resistance to chemotherapy was noted.[10] Therefore, extending the line of reasoning that surgery affords the best chance of cure would lead one to advocate a complete bilateral dissection, including nodes in the suprahilar regions, for patients with suspicious nodes.
Recognition of associated morbidity and clinical experience with modern chemotherapeutic protocols have allowed us to move away from this historical approach. Whether the refractory phenotype is acquired or inherent is unknown. The National Cancer Institute intergroup study demonstrated that the relapse rate in patients with positive lymph nodes can be substantially reduced with a short course of chemotherapy.[11] Therefore, several centers, including ours, advocate the use of adjunctive chemotherapy in patients with pathologic stage II disease following either open or laparoscopic lymphadenectomy.
Does Laparoscopic Retroperitoneal Lymphadenectomy Have Therapeutic Benefits?
Concerns exist regarding the therapeutic benefits of laparoscopic retroperitoneal lymph node dissection. In reviewing currently available series, no recurrences have been reported in the retroperitoneum.[3-6] Moreover, among patients with positive nodes, no retroperitoneal recurrences have been identified. Although a similar number of nodes can be removed from well-established templates with the laparoscopic approach as with open surgery, longer follow-up in larger series will be required to make definitive therapeutic claims.
Conclusions
Data support the contention that laparoscopic retroperitoneal lymph node dissection provides pathologic staging information in patients with clinical stage I nonseminomatous germ-cell tumors. This information allows for a more rational assignment of individual patients to surveillance or systemic chemotherapy. The laparoscopic procedure, although technically demanding, is feasible. Longer follow-up is needed to assess its therapeutic efficacy. Therefore, current application of laparoscopic retroperitoneal lymph node dissection is determined by one’s philosophy in treating testes cancer.
When chemotherapy is given as an adjunct in patients with pathologic stage II disease, laparoscopy can avoid the morbidity associated with open retroperitoneal lymphadenectomy. Let us not forget that any form of surgery carries postoperative discomfort and risks.
Research efforts should focus on seeking a reliable predictor of the biological behavior of each patient’s tumor. With the development of noninvasive markers (ie, markers of true pathologic staging) and the evolution of alternative therapeutic regimens, the need for lymphadenectomy will someday be only of historical interest.
References:
1. Ratner LE, Montgomery RA, Kavoussi LR: Laparoscopic live donor nephrectomy: The 4-year Johns Hopkins University experience. Nephrol Dial Transplant 14:2090-2093, 1999.
2. Bauer JJ, Bishoff JT, Moore RG, et al: Laparoscopic vs open pyeloplasty: Assessment of objective and subjective outcome. J Urol 162:692-695, 1999.
3. Janetschek G, Hobisch A, Holti L, et al: Retroperitoneal lymphadenectomy for clinical stage I nonseminomatous testicular tumors: Laparoscopic vs open surgery and impact of learning curve. J Urol 156:89-93, 1996.
4. Gerber GS, Bissada NK, Hulbert JC, et al: Laparoscopic retroperitoneal lymphadenectomy: Multi-institutional analysis. J Urol 152:1188-1191, 994.
5. Nelson JB, Chen RN, Bishoff JT, et al: Laparoscopic retroperitoneal lymph node dissection for clinical stage I nonseminomatous germ-cell testicular tumors. Urology, 1999 (in press).
6. Rassweiler JJ, Seemann O, Henkel TO, et al: Laparoscopic retroperitoneal lymph node dissection for nonseminomatous germ-cell tumors: Indications and limitations. J Urol 156:1108-1113, 1996.
7. Winfield HN, Donovan JF, See, et al: Laparoscopic pelvic lymph node dissection for genitourinary malignancies: Indications, techniques, and results. J Endourol 6:103-111, 1992.
8. Chi DS: Laparoscopy in gynecologic malignancies. Oncology 13:773-782, 1999.
9. Donohue JP, Thornhill JA, Foster RS, et al: Primary retroperitoneal lymph node dissection in clinical stage A nonseminomatous germ-cell testis cancer: Review of Indiana University experience 1965-1989. Br J Urol 71:326-335, 1993.
10. Baniel J, Foster RS, Einhorn, LH, et al: Late relapse of clinical stage I testicular cancer. J Urol 154:1370-1372, 1995.
11. Williams SD, Stablein DM, Einhorn LH, et al: Immediate adjunctive chemotherapy vs observation with treatment at relapse in pathological stage II testicular cancer. N Engl J Med 317:1433-1438, 1987.
Articles in this issue
about 26 years ago
Off-Label Drug Promotionabout 26 years ago
Clinton Medical Records Privacy Proposalabout 26 years ago
Book Review:Pediatric Hematology, Second Editionabout 26 years ago
Women Are Replacing Old Breast Implants With Newabout 26 years ago
FTC Warns Against Home-Use Tests for HIVNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.