- ONCOLOGY Vol 14 No 11
- Volume 14
- Issue 11
HCFA Backs Off of Reimbursement Cuts for Oncology Drugs
The Health Care Financing Administration (HCFA) sent a letter to Medicare insurance carriers in September telling them not to cut reimbursement to oncologists for 14 oncology drugs that are administered in the oncologist’s office. This was a reversal of what HCFA said it planned to do, based on pricing data developed by the US Justice Department. Those data showed that drug manufacturers were reporting “average wholesale prices” (AWPs) to Medicare for those 14 drugs that were much higher than the actual AWPs. Medicare reimburses the oncologist for 95% of the AWP. The Justice Department alleges that the drug companies report a very high AWP and then actually sell the drug to the oncologist for a considerably lower price, allowing the oncologist to make a tidy profit after Medicare reimburses at the higher price. The American Society of Clinical Oncology (ASCO) argued that Medicare woefully under-reimburses oncologists for chemotherapy administration, and, therefore, any additional revenue the doctors can generate via AWP reimbursements is warranted. ASCO took that argument to Capitol Hill, and legislators brought pressure to bear on HCFA administrator Nancy-Ann Min DeParle. “We would like to acknowledge HCFA’s willingness to work with the cancer community on this important issue,” said Lawrence H. Einhorn, MD, president of ASCO. Of equal importance is DeParle’s commitment to increase practice expenses for the CPT codes for chemotherapy administration. That will be done in the summer of 2001, when HCFA publishes a proposed Medicare fee schedule for calendar year 2002.
The Health Care Financing Administration (HCFA) sent a letter to Medicare insurance carriers in September telling them not to cut reimbursement to oncologists for 14 oncology drugs that are administered in the oncologists office. This was a reversal of what HCFA said it planned to do, based on pricing data developed by the US Justice Department. Those data showed that drug manufacturers were reporting average wholesale prices (AWPs) to Medicare for those 14 drugs that were much higher than the actual AWPs. Medicare reimburses the oncologist for 95% of the AWP. The Justice Department alleges that the drug companies report a very high AWP and then actually sell the drug to the oncologist for a considerably lower price, allowing the oncologist to make a tidy profit after Medicare reimburses at the higher price. The American Society of Clinical Oncology (ASCO) argued that Medicare woefully under-reimburses oncologists for chemotherapy administration, and, therefore, any additional revenue the doctors can generate via AWP reimbursements is warranted. ASCO took that argument to Capitol Hill, and legislators brought pressure to bear on HCFA administrator Nancy-Ann Min DeParle. We would like to acknowledge HCFAs willingness to work with the cancer community on this important issue, said Lawrence H. Einhorn, MD, president of ASCO. Of equal importance is DeParles commitment to increase practice expenses for the CPT codes for chemotherapy administration. That will be done in the summer of 2001, when HCFA publishes a proposed Medicare fee schedule for calendar year 2002.
Articles in this issue
over 25 years ago
Clinical Oncology, Second Editionover 25 years ago
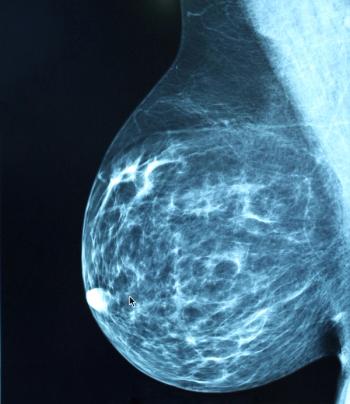
Early Diet May Play Important Role in Breast Cancer RiskNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.