
Oncology NEWS International
- Oncology NEWS International Vol 9 No 5
- Volume 9
- Issue 5
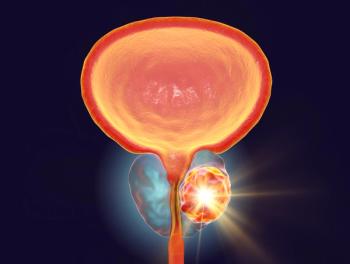
NCCN Prostate Cancer Practice Guidelines Revised
FT. LAUDERDALE, Fla-Slight changes in the administration of salvage therapy after radical prostatectomy are among several revisions to the National Comprehensive Cancer Network (NCCN) Practice Guidelines for Prostate Cancer. The revised guidelines recommend radiotherapy for men with positive margins whose prostate-specific antigen (PSA) levels fail to fall to 0 ng/mL after surgery.
FT. LAUDERDALE, FlaSlight changes in the administration of salvage therapy after radical prostatectomy are among several revisions to the National Comprehensive Cancer Network (NCCN) Practice Guidelines for Prostate Cancer. The revised guidelines recommend radiotherapy for men with positive margins whose prostate-specific antigen (PSA) levels fail to fall to 0 ng/mL after surgery.
In a more controversial recommendation, the guidelines also urge physicians to consider radiotherapy in men with negative margins whose PSA levels fail to fall to 0 ng/mL. Sequential androgen ablative therapy is recommended after salvage therapy.
With negative margins, if the PSA does not drop to 0 at a predetermined time, usually 3 months after surgery, one should consider adjuvant radiotherapy, even though we all realize this is very controversial, said Julio Pow-Sang, MD, professor of surgery, University of South Florida. Failure of the PSA to drop to 0 often indicates metastatic disease, he said.
The panel went ahead with the recommendation even as it anxiously awaits the Southwest Oncology Group (SWOG) randomized study of adjuvant radiotherapy in high-risk patients, he said.
Dr. Pow-Sang and Howard Sandler, MD, of the University of Michigan Comprehensive Cancer Center, and chair of the RTOG genitourinary committee, presented the revisions to the NCCN guidelines at the Fifth Annual NCCN conference. Lawrence Baker, DO, of the University of Michigan Comprehensive Cancer Center, chaired the prostate cancer guidelines panel.
For men with a rising PSA after radical prostatectomy, the guidelines offer several pathways for salvage workup and therapy, but many choices are left to the discretion of the physician. For instance, bone scan, biopsy, and ProstaScint (immunoscintigraphy) are all presented as tests physicians may wish to consider, but none is explicitly recommended.
When there is an indication of biochemical failure, there is not much concordance about when these tests should be done, Dr. Pow-Sang said. Most of the literature is not very clear about the value of tests.
As with the previous version of the guidelines, three options for salvage therapy for these patients are endorsed: radiotherapy, androgen ablation, or observation. However, in the most recent version of the guidelines, radiotherapy is presented as the preferred option if PSA levels rise 1 year or more after surgery, the seminal vesicle is not involved, the Gleason score is less than 8, and the PSA level is below 2 ng/mL.
The data over the last several years show that radiotherapy is less effective when the PSA levels are more than 2.5 ng/mL, Dr. Pow-Sang said. So we set a limit of 2 ng/mL as the guideline for when to use salvage radiotherapy.
Asymptomatic Men
Other changes to the guidelines include the addition of a second treatment option for men who are asymptomatic upon diagnosis and have a life expectancy of less than 5 years.
Previous guidelines for this group recommended only that no further workup be done until symptoms occurred. However, the newly revised guidelines urge physicians to consider radiotherapy for some men in this group, depending upon stage, Gleason score, PSA, and patient characteristics.
This was inserted into the guidelines to allow for radiation therapy in patients who would be expected to develop symptoms or have relatively aggressive cancers even though their life expectancy might be relatively short, Dr. Sandler said. This is expected to be a relatively small subset of patients.
Risk Categorization
The risk categorization for men with localized disease has also been revised somewhat. Previous guidelines defined risk of progression based on clinical stage and Gleason score. The guidelines now distinguish between very low risk and low risk, based on the amount of tumor in the biopsy specimen. Less than 5% of tumor in the specimen is considered very low risk. Emerging evidence demonstrates that the amount of disease in the specimen is independently prognostic of progression, Dr. Sandler said.
Although the NCCN panel chose to express the amount of tumor in the specimen as a percentage, that is not the only way to measure the presence of disease. Its unclear exactly how best to quantify that, Dr. Sandler said. Some people calculate tumor presence based on the number of cores that are positive, while others measure it as the percentage of involvement in the entire specimen.
Articles in this issue
almost 26 years ago
HRT Not Associated with Lower Survival After Breast Canceralmost 26 years ago
Age No Contraindication to High-Dose Therapy in Myelomaalmost 26 years ago
ASCO Urges Passage of Patient’s Bill of Rightsalmost 26 years ago
RT Not Necessarily an Impedance to Breast Reconstructionalmost 26 years ago
New Adjunctive Regimens for Breast Cancer Treatment Are Under Studyalmost 26 years ago
ERT Does Not Increase Endometrial Cancer Recurrencealmost 26 years ago
Radiochemotherapy/Transplant in Low-Grade Lymphomasalmost 26 years ago
Fish Oil Supplements May Improve Cancer Therapies’ Effectivenessalmost 26 years ago
Study of Dying Cancer Patients Reveals Importance of Ritualsalmost 26 years ago
Treatment of Brain Metastases Called an ‘Orphan Specialty’Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.
Related Content


PSMA PET/CT–Guided Radiation Exhibits Favorable Prostate Cancer Outcomes








































