Articles by E. David Crawford, MD

ONCOLOGY® editorial board member E. David Crawford, MD, and colleagues, propose a new model for guiding the treatment of prostate cancer that focuses on a “transitional state,” which occurs during the interval of progression to metastatic castration-resistant prostate cancer.
Experts discuss the case of a 69-year-old man with a history of metastatic prostate cancer previously treated with androgen deprivation therapy with leuprolide.
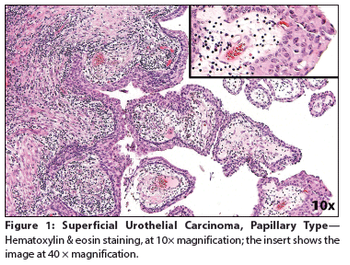
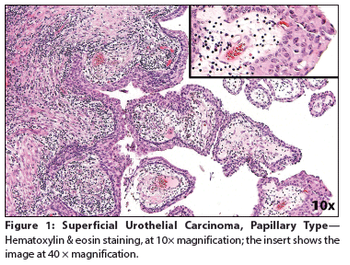
Lymphoepithelioma-Like Carcinoma of the Urinary Bladder
ByElizabeth R. Kessler, MD,Arya Amini, MD,Shandra S. Wilson, MD,Kathryn Breaker, RN-MS, ANP-C,David Raben, MD,Francisco G. La Rosa, MD,E. David Crawford, MD A 65-year-old woman presented to a local emergency department complaining of right flank pain that had worsened over the past 10 days. A CT scan of the abdomen and pelvis showed intravesical tumors of the urinary bladder.
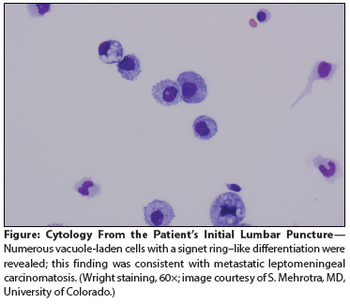
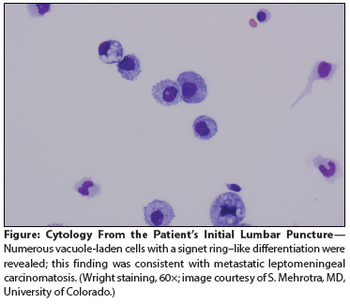
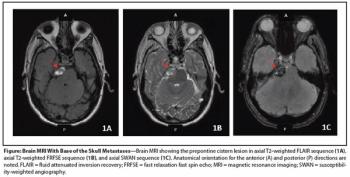
A 59-year-old man with metastatic gastric cancer presented to the oncology clinic with a 1-week history of positional headache, nausea, and vomiting. He stated that the headache was located in the frontal region, was 8 on a scale of 10 in intensity.
This article reviews recent evidence suggesting an increased risk of pneumonia, cardiovascular disease, and acute kidney injury in men treated with ADT and consider whether the incidence of such events differs with the treatment modality.
A 63-year-old man with no family history of prostate cancer has prostate biopsy that revealed 9 out of 12 cores involved with prostatic adenocarcinoma, mostly Gleason score 5+4=9.
We briefly review these two imaging technologies and provide potential utilization strategies based on available data.

In the past 5 years we have taken at least 7 steps forward for men with prostate cancer-which hopefully will turn into “one giant leap” in our attempt to convert advanced prostate cancer into a chronic disease.
In this article, we review recent advances in the discovery of prostate cancer biomarkers, their integration into clinical practice, and implications for improving clinical management of the disease.

A 46-year-old man sought consultation for an abnormal prostate-specific antigen (PSA) level of 9 ng/mL and one prior negative biopsy. Five months ago, while traveling, he had presented to an urgent care facility with a 24-hour history of fever, chills, nausea, and vomiting.

We have entered a period of accelerated drug development and optimism in the care of advanced prostate cancer. The treatment paradigm for these patients is rapidly evolving, with future study needed to define the optimal sequencing and potential combinations of these new agents.

This review will examine agents with potential activity in the palliation and treatment of skeletal metastases of prostate cancer, and will weigh the clinical-outcomes evidence for and against their broad use.

This article will present a detailed review of the body of evidence regarding the PSA assay, with reflections on the resulting future of prostate cancer screening.

The patient is a 26-year-old woman with a complex oncologic history. At 1 year of age, she was diagnosed with a stage III abdominal neuroblastoma, which was treated, and again at age 9, she had a recurrence of neuroblastoma in the left axilla. She was in her usual state of good health until 18 months ago, when she presented with hematuria and was found to have a right-sided kidney mass.

More than 50% of patients with advanced breast or prostate cancer have identifiable bone metastasis, and 30% to 40% of patients with non–small-cell lung cancer ultimately develop metastases to bone.[1,2]

Physicians have known since 1941 that testosterone suppression benefits patients with symptomatic metastatic prostate cancer.[1] The pioneering study in this regard showed that estrogen therapy achieved comparable efficacy to castration by improving acid and alkaline phosphatase levels associated with relief of cancer-related symptoms. More than 6 decades later, however, many of the therapies subsequently developed for achieving androgen deprivation still suffer from serious limitations.

The article by Polascik and coauthors provides a timely synopsis of modern technologic advances in prostate cryoablation and a review of the rationale for and experience with targeted prostate treatments. Prostate cryoablation has a storied past, which can be briefly summarized as high excitement followed by near-complete abandonment. Fortunately, a few practitioners improved the technique and incorporated new technologies allowing for its resurrection.

The patient is a 39-year-old Caucasian male who presented with a right renal mass and painless gross hematuria. He underwent a right laparoscopic radical nephrectomy and the final pathology revealed a carcinoid tumor.

Prostate Cancer in a Man With Multiple Previous Cancers
ByThomas Flaig, MD,E. David Crawford, MD,Brian Kavanagh, MD,Scott Lucia, MD,Francisco G. La Rosa, MD,Al Barqawi, MD,Frances Crighton, RN, MSN, PhD,L. Michael Glodé, MD, FACP patient is a 67-year-old male with mild obstructive symptoms and an American Urology Association symptom score of 8.[1] He was noted to have a prostate-specific antigen (PSA) level of 3.2 ng/mL. Because this represented a significant increase in his PSA velocity (rate of change over time), he proceeded to have a biopsy, which was positive for prostate cancer. He has no other complaints and visits us for an opinion on the treatment of his prostate cancer.

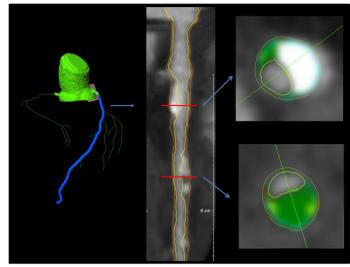
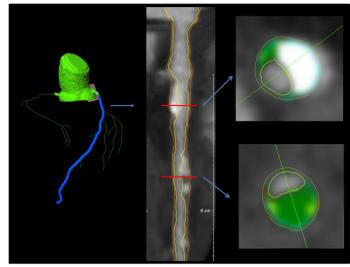
The morbidities associated with prostate cancer treatments have improved over the years. However, potential overtreatment and the risks of adverse events associated with radical treatment still pose a considerable challenge. Targeted focal therapy (TFT) of prostate cancer appears to be part of a logical continuum in the quest to improve upon the management of early organ-confined disease. TFT is a procedure in which only the cancer in the gland is ablated. The normal gland, sphincter, and in most cases the neurovascular bundles are preserved. Therefore, this approach averts some of the common complications of more radical therapy. Initial experience has been encouraging; however, long-term data and full implementation of emerging advances in imaging are urgently needed before the widespread adoption of this approach. In this review, we present the current status of our knowledge about this procedure and the most important challenges that need to be addressed. We also present the initial results with this approach at our center.

Arguably the most important step in the prognosis of prostate canceris early diagnosis. More than 1 million transrectal ultrasound (TRUS)-guided prostate needle biopsies are performed annually in the UnitedStates, resulting in the detection of 200,000 new cases per year. Unfortunately,the urologist's ability to diagnose prostate cancer has not keptpace with therapeutic advances; currently, many men are facing theneed for prostate biopsy with the likelihood that the result will beinconclusive. This paper will focus on the tools available to assist theclinician in predicting the outcome of the prostate needle biopsy. We willexamine the use of "machine learning" models (artificial intelligence),in the form of artificial neural networks (ANNs), to predict prostatebiopsy outcomes using prebiopsy variables. Currently, six validatedpredictive models are available. Of these, five are machine learningmodels, and one is based on logistic regression. The role of ANNs inproviding valuable predictive models to be used in conjunction withTRUS appears promising. In the few studies that have comparedmachine learning to traditional statistical methods, ANN and logisticregression appear to function equivalently when predicting biopsyoutcome. With the introduction of more complex prebiopsy variables,ANNs are in a commanding position for use in predictive models. Easyand immediate physician access to these models will be imperative iftheir full potential is to be realized.

Hormonal treatment of advanced prostate cancer should be consideredfor patients who have stages C and D1 disease, a high risk of recurrenceafter local therapy, or prostate-specific antigen–measured recurrenceafter local treatment. This approach is dependent on most prostatecancer cells being androgen-dependent, but androgen-independentcells may arise after several years of hormonal therapy. Options forandrogen blockade primarily include orchiectomy, luteinizing hormone–releasing agonists and antagonists, and nonsteroidal antiandrogens.There is some controversy regarding combined androgen blockade,intermittent androgen blockade, and the question of whether earlyandrogen blockade is superior to delayed therapy. Convincing data doexist for the use of adjuvant/neoadjuvant hormonal therapy with external-beam radiation therapy. Although hormonal therapy is an importanttreatment modality for advanced prostate cancer, long-termtreatment carries significant side effects that need to be considered.

As a tumor marker, prostate specific antigen (PSA) has revolutionized the detection and management of adenocarcinoma of the prostate. From its discovery in the early 1970s to its application in the 1980s and finally widespread use in the 1990s, PSA has profoundly affected the way in which we treat prostate cancer. Many researchers in basic science and clinical practice have helped to create the PSA story, and the authors of this manuscript have made major contributions to our understanding of PSA as a tumor marker.

A 72-Year-Old Man With Prostate Cancer
ByCraig Berman, MD,Marcus Chen, MD,E. David Crawford, MD,Frances Crighton, RN, MSN, PhD,Marshal Freeman, MD,L. Michael Glodé, MD, FACP,Andrew Kraft, MD,Scott Lucia, MD,David Raben, MD The patient, L.E., is a 72-year-old white male who has been under our care for 10 years. He initially presented to our clinic in 1992, with a diagnosis of localized prostate cancer.

Over the past several years, the clinical presentation of prostate cancer has evolved so that more patients than ever before are presenting with clinically localized disease. However, a significant number of men continue to

Erectile dysfunction is a common occurrence as men age. Approximately 20% of men over the age of 50 years report difficulty in achieving or maintaining an erection, and as many as 60% of men age 70 and older suffer from erectile dysfunction.[1]

Dr. Moul discusses one of the most contemporary yet contrversial topics in prostate cancer-namely, a rising prostate-specific antigen (PSA) level after the failure of local therapy. The way in which patients with advanced prostate cancer present

Prostate Cancer Clinical Trials of the Southwest Oncology Group
ByE. David Crawford, MD,Edward P. Deantoni, PhD,Maha H. Hussain, MD,Ian M. Thompson, Jr, MD,Charles A. Coltman, Jr, MD The changing clinical dynamics of prostate cancer have resulted in a broadening of the research focus of the Genitourinary (GU) Cancer Committee of the Southwest Oncology Group (SWOG). Beginning with an emphasis on hormone-refractory disease in its early years, SWOG prostate cancer trials now cover the entire spectrum of the disease: localized, locally advanced, metastatic and hormone-refractory disease. As the world's largest GU cancer research group, the GU committee of SWOG has pioneered studies in combined androgen therapy for metastatic disease, quality-of-life (QOL) assessments for patients with localized and advanced disease, adjuvant therapy models, and prostate cancer chemoprevention. The committee has also formed the GU Global Group, whose purpose is to convene the chairs of the GU committees of all the major national and international oncology cooperative groups. Meeting semiannually, this group discusses activities within their respective organizations, plans collaborative strategies and protocols, and establishes global strategy in prostate cancer clinical research. The future directions of national and international prostate cancer trials will build on this broad foundation of well-conceived, logically sequenced studies. [ONCOLOGY 11(8):1155-1170, 1997]

Controversy exists over the optimal management of patients with an asymptomatic rising prostate-specific antigen (PSA) following definitive therapy for clinically localized prostate adenocarcinoma.

During the past decade, there has been an increase of over 300% in the incidence of prostate cancer and a 150% increase in the death rate from this dreaded cancer. It is estimated that more than 244,000 men will be diagnosed with this neoplasm during 1995, and at least 42,000 will die as a direct result of the disease [1]. Challenged by this dramatically rising incidence and mortality, three strategies can be implemented: (1) attempt to prevent the disease; (2) find the disease early, treat it, and cure it; and (3) discover a cure for the disease once it has escaped the bounds of the prostate.