Articles by Greg Frieherr

Research from Japan documenting remarkable survival rates among patients with inoperable lung cancer may only hint at the potential of proton-beam radiation therapy. The study out of the Proton Medical Research Center in Tennoudai, Japan, documented high survival rates for 55 patients suffering from stage I inoperable non-small-cell lung cancer.
The key to effective treatment of squamous lung cell lung cancer in smokers may be at hand.

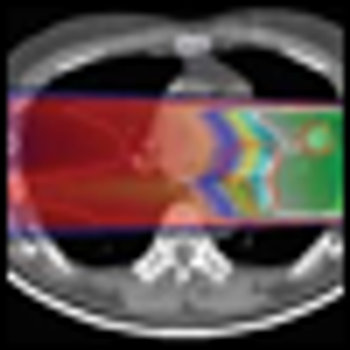
A new hybrid technology emerged at radiology’s mega conference in Chicago earlier this month, one that may dislodge decade-old PET/CT from its prominent berth for the diagnosis and monitoring of cancer patients. This new modality combines the positron-imaging component of PET/CT with oncology’s premier anatomic modality, MR, opening the door to cancer images with unprecedented clarity and clinical value.

Pathologies such as infections, or even tumors, crop up from time to time in patients examined for entirely unrelated issues. These "incidental findings"can put doctors-and patients-in a tight spot. How do they proceed with the patient, knowing that many of the asymptomatic signs of disease may never lead to clinical problems, or may simply be false positives?

The search for a magic bullet against cancer historically has glowed bright then dimmed, depending on the stage of discovery. Developments surrounding monoclonal antibodies and angiogenesis inhibitors have followed this cycle, as exuberance for their potential has bowed to the nuances that underlie the complex mechanisms on which they depend.

McKesson plans to spend more than $2 billion to purchase the largest community-based cancer treatment and research network in America.
Research from Japan documenting remarkable survival rates among patients with inoperable lung cancer may only hint at the potential of proton beam therapy.

Cancer care experts describe the building blocks for creating a survivorship program.

The search for a magic bullet against cancer historically has glowed bright then dimmed, depending on the stage of discovery. Developments surrounding monoclonal antibodies and angiogenesis inhibitors have followed this cycle, as exuberance for their potential has bowed to the nuances that underlie the complex mechanisms on which they depend.

On average, 11% of cancer patients drop out of hospice care, according to research conducted at the Mount Sinai School of Medicine. Many of these patients are in for rough sledding.

Patients are beating cancer only to fall prey to sexual dysfunction, body pain, and chronic disease. The physical symptoms of their success increase the emotional burden, leading to anxiety, depression, and even suicide, as they are reminded daily of the chance that the cancer they had might return or a new one might occur.

Earlier this month two senators introduced the “Consistency, Accuracy, Responsibility, and Excellence in Medical Imaging and Radiation Therapy Act of 2010.” Sens. Mike Enzi (R-Wyo.) and Tom Harkin (D-Iowa) hope through this legislation to guarantee that staff who perform medical imaging and radiation therapy are appropriately qualified by establishing standards for these personnel. It makes sense. Who wants unqualified personnel performing procedures involving ionizing radiation?

Clinical studies examining the potential of CT exposure to cause cancer are under way, but it could be years or even a decade until the results are known, and even then, they may be inconclusive.

A flood of cancer-specific applications is answering the call of oncologists, for whom keeping pace with new clinical developments is a higher priority than for your average family practitioner.

There was a time when a cancer diagnosis meant long commutes for patients in small communities and rural America. The kind of care they needed was available only at tertiary medical centers, typically in metropolitan areas. An expanded network of community cancer clinics changed that, providing convenience and comfort for many thousands of patients. A few years ago those centers were treating four out of five U.S. cancer patients. But now this net of care providers is collapsing under the weight of falling Medicare reimbursement.

Go back to the beginning of MRI, in the early and mid-1980s, and you’ll find an almost rabid adoption of the modality, despite scant evidence of its clinical value. MRI has since done much to gain the trust of the medical community, opening a diagnostic cornucopia in the process. But the future has to bring more if MR is going to extend this legacy. Researchers at Wake Forest University Baptist Medical Center are working on it.
Like satellites tracking an invading force, a PET scanner at UCLA follows a battalion of tumor-seeking lymphocytes stalking melanoma tumors. Radioactive reporter genes, embedded in the lymphocytes, show the real-time location of these immune cells, genetically engineered to recognize antigens on the surface of the tumor cells.

Multiple scans are now par for the course in cancer care. Experts debate whether all are essential to patient management or some should be cut to help rein in surging costs.

They are nearly microscopic, yet ganged together they can pack a big punch. They are microbeads embedded with radioisotopes and infused into body parts containing cancer tumors. The idea is to surround and destroy the tumor. The problem is making sure the microbeads stay put. SPECT/CT can provide the information to make it work.

Go back to the Eisenhower years and amid the gray flannel suits, rabid McCarthyism, and dread over nuclear war you’ll find rays of hope in the battle against cancer. Looking back from the 60s, it was easy to believe that this hope was unfounded, an unwarranted faith engendered by the conquest of polio. But it may have been that science simply was not ready.

Radiologists have come to expect rising demand for CT, which is why anecdotal reports of sudden and dramatic falls in CT volumes have sent a shudder through the community. All the more alarming is that the rumored drop-offs are coming at the request of patients who want nothing to do with CT because they fear its radiation will someday cause cancer. Instead they reportedly are demanding ultrasound or MRI because neither has ionizing radiation -- never mind that neither is indicated, nor, particularly in the case of ultrasound, has much chance of providing useful information.

Typically glioblastoma patients are dead within 15 months of diagnosis, no matter how complete and well-planned their therapy.

The I-SPY 2 breast cancer trial features a novel design of uninterrupted enrollment and patient stratification using biomarkers in order to target therapy.

Medical imaging represents “low-hanging fruit” in the battle to curtail rising cancer costs, according to Dr. Kevin Schulman, director of the Duke Center for Clinical and Genetic Economics at Duke University.

Typically glioblastoma patients are dead within 15 months of diagnosis, no matter how complete and well-planned their therapy. Cells sloughed from the brain tumor escape the surgery and somehow stand up to months of radiation and chemotherapy, leading to a recurrence of the tumor and the death of the patient. Researchers at the University of Bonn are beginning to unwind how they do it.

African Americans have a higher mortality rate from lung cancer than Caucasians, a fact first discovered in the early 1980s. For decades, researchers have looked for differences in access to care, rates of surgery, and patient preferences to explain the disparity. Now it seems the answer may relate at least partly to the way African Americans think about lung cancer.

Cancer will kill more than a half million people in this country this year. Many will not go quietly. Their diseased hearts, impaired further by a losing battle against cancer, will shut down only to be shocked back to life by implanted defibrillators that could have been turned off but were not.

The regimented and inflexible protocols that have long served as hallmarks of clinical trials are giving way to personalized medical research. A clinical trial begun last week at the University of California, San Francisco will use genetic and biological markers drawn from the tumors of individual patients to identify the treatments most likely to be effective for those participating in the trial.

For quality to become the standard, care delivery must be fundamentally changed and oncologists will need to step up to work with insurance providers.

News that President Obama received a clean bill of health from a virtual colonoscopy several days ago rubbed influential gastroenterologists the wrong way.