
Theranostics, a technique that combines traditional medication with diagnostics, is “limitless”, according to Brandon Mancini, MD, MBA, FACRO.

Your AI-Trained Oncology Knowledge Connection!


Theranostics, a technique that combines traditional medication with diagnostics, is “limitless”, according to Brandon Mancini, MD, MBA, FACRO.

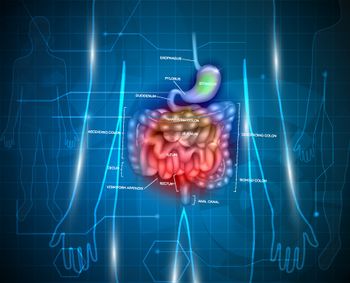
According to investigators of the phase 3 SCOT trial, most patients with colon and rectal cancer should be receiving only 3 months of adjuvant treatment.

One of the lesser-known costs of undergoing cancer treatment is the loss of work opportunities, according to Loretta Nastoupil, MD.

People who consumed 14 or more drinks per week experienced a higher risk of colorectal cancer compared with those who consumed one or fewer drinks.
Anbenitamab plus chemotherapy reduced the risk of progression or death by 75% vs chemotherapy alone in select patients with gastric cancer/gastroesophageal adenocarcinoma.

With a median follow-up of 6 months, the median OS was not yet reached in patients with recurrent glioblastoma with the nogapendekin alfa inbakicept-based regimen.

Data from the phase 3 BREAKWATER trial demonstrated that encorafenib plus cetuximab and chemotherapy yields clinical benefit for this patient population.

Treatment with relacorilant plus nab-paclitaxel yielded a 35% reduction in the risk of death compared with nab-paclitaxel alone for patients with platinum-resistant ovarian cancer.

Bezuclastinib plus sunitinib yielded favorable PFS and ORR data vs sunitinib alone in patients with previously treated gastrointestinal stromal tumors.
Data from 2 trials at the 2024 and 2025 ASCO Annual Meetings demonstrate the PD-L1/4-1BB bispecific antibody’s efficacy and safety in this population.

The folate receptor α ADC yielded responses, with a favorable safety profile, in patients with high-grade serous ovarian cancer in a phase 1 trial.

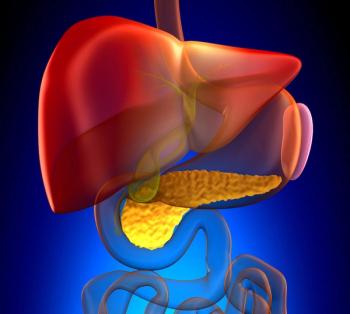
Patients with pancreatic cancer who received up to 6 infusions of the multiantigen-targeted T cell product only experienced 1 treatment-related serious AE.

Patients with HER2-mutant NSCLC who were naïve to systemic therapy for advanced disease experienced positive results following treatment with sevabertinib.
Results from the phase 3 VERIFY and phase 2 REVIVE studies supported the NDA submission of the for rusfertide in this PV patient population.
The majority of patients with de novo DLBCL who received zanubrutinib plus rituximab and lenalidomide achieved complete responses in a phase 2 trial.

Olvimulogene nanivacirepvec yielded 3 partial responses among 9 evaluable patients with SCLC who had progression or recurrence on prior therapy.
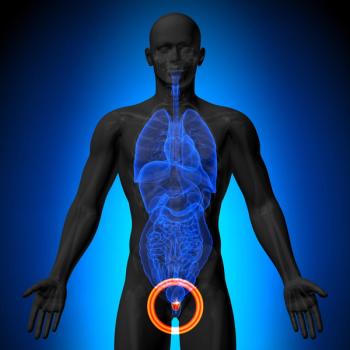
Patients with low-risk prostate cancer who have a BMI of 30 or greater experienced a potentially harmful effect after receiving metformin.

Stereotactic body radiotherapy alone may be feasible instead of immediate systemic therapy in select patients with oligometastatic cancer.
Nurses preferred the FreedomEDGE infusion system compared with the manual push technique in a retrospective survey study.
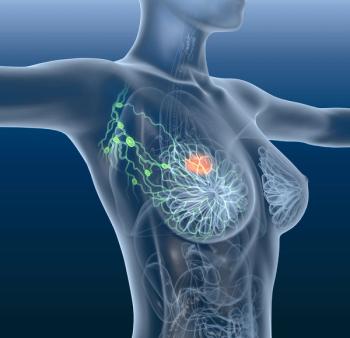
Results from the DESTINY-Breast05 trial revealed that T-DXd was superior to T-DM1 in these patients with HER2-positive early breast cancer.

OncoPrism-NSCLC was found to be a predictive biomarker of immune checkpoint inhibitor benefit vs a general prognostic tool in patients with NSCLC.
BGB-B2033 is under evaluation for patients with hepatocellular carcinoma who progressed on or after systemic therapy in a first-in-human phase 1 trial.
Fuzuloparib monotherapy and as a combination with apatinib improved PFS as maintenance therapy in patients with ovarian cancer harboring BRCA1/2 mutations.

Among the 12 patients with suspected brain metastases treated with RAD 101, the images showed metabolic activity in brain metastases compared with MRI findings.

The decision is based on results from the phase 3 MajesTEC-3 trial, which showed a PFS benefit with the teclistamab combination in patients with pretreated multiple myeloma.

Results from the phase 3 DESTINY-Breast09 trial led to the approval of T-DXd plus pertuzumab in unresectable/metastatic HER2+ breast cancer.

Alan Pliskin and Mary Kay Yamamoto discuss their journey through multiple myeloma treatment, emphasizing the importance of knowledge, positivity, and quality of life.
Results from the ARTEMIS-001 trial previously showed that the B7-H3–targeted ADC elicits deep responses in patients with ES-SCLC.
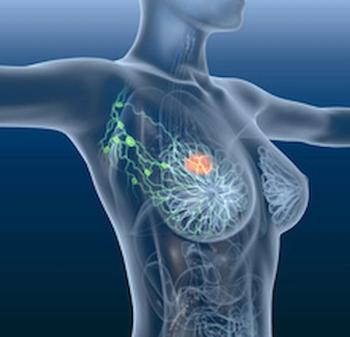
The 60-month local regional recurrence-free rate was 93.2% in the MRI arm vs 95.7% in the no MRI arm among patients with newly diagnosed breast cancer.

Patients with SCLC who received ociperlimab and tislelizumab plus cCRT achieved a median PFS of 12.6 months compared with 9.5 months with cCRT alone.

Published: May 5th 2025 | Updated:

Published: April 8th 2025 | Updated:

Published: October 14th 2025 | Updated:

Published: May 1st 2025 | Updated:

Published: August 5th 2025 | Updated:
Published: September 26th 2025 | Updated: