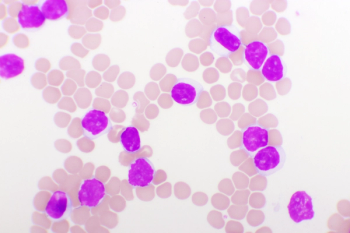
Matthew S. Davids, MD, MMSc, spoke about the benefit of venetoclax combinations in patients with chronic lymphocytic leukemia or small lymphocytic lymphoma.

Your AI-Trained Oncology Knowledge Connection!

Matthew S. Davids, MD, MMSc, spoke about the benefit of venetoclax combinations in patients with chronic lymphocytic leukemia or small lymphocytic lymphoma.
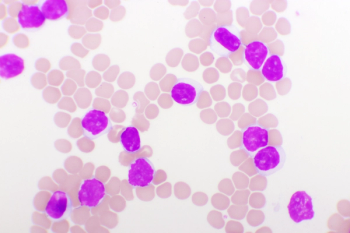
Lindsey Roeker, MD, spoke about identifying the correct population of patients with chronic lymphocytic leukemia who will benefit from umbralisib and ublituximab plus ibrutinib.
Matthew S. Davids, MD, MMSc, spoke about using venetoclax plus acalabrutinib in the phase 3 MAJIC study for patients with chronic lymphocytic leukemia or small lymphocytic lymphoma.
Lindsey Roeker, MD, spoke about phase 2 trial results which demonstrated efficacy of the combination of umbralisib and ublituximab added to ibrutinib for patients with chronic lymphocytic leukemia.
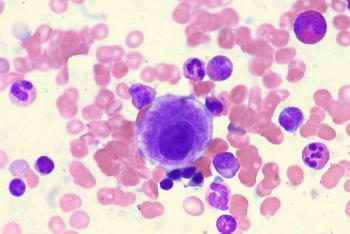
The combination of acalabrutinib, with or without obinutuzumab, produced a strong survival benefit for patients with treatment-naïve chronic lymphocytic leukemia over treatment with ibrutinib or venetoclax plus obinutuzumab.
Preclinical evidence supports further research in combining a menin inhibitor plus targeted therapies, as this may result in superior efficacy for patients with KMT2A-rearranged and NPM1-mutated acute myeloid leukemia.
Lindsey Roeker, MD, spoke about using a combination that includes a Bruton tyrosine kinase inhibitor, PI3K inhibitor, and an anti-CD20 monoclonal antibody for patients with chronic lymphocytic leukemia.
A non inferiority design was presented at ASH 2021 for acalabrutinib plus venetoclax in treatment-naive chronic lymphocytic leukemia or small lymphocytic leukemia.

Jennifer A. Woyach, MD, spoke about why it’s important to use newer therapies instead of chemoimmunotherapy for patients with chronic lymphocytic leukemia.

Maintenance oral azacitidine produced a sustained survival benefit over placebo for patients with acute myeloid leukemia in first remission.

Jennifer A. Woyach, MD, spoke about the results of a study conducted in elderly patients treated with an ibrutinib-containing regimen for chronic lymphocytic leukemia at 55 months of follow-up.
The combination of high-frequency and low-dose acalabrutinib and rituximab demonstrated a 100% overall response rate in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma.

Acalabrutinib produced positive quality-adjusted survival benefits over other treatment options for patients with relapsed/refractory chronic lymphocytic leukemia.

A post-hoc analysis of a phase 3 trial presented at 2021 ASH indicate that acalabrutinib may be favorable in terms of toxic burden and cardiovascular-related events when compared against ibrutinib for treating chronic lymphocytic leukemia.

A phase 2 study has begun recruiting patients with relapsed/refractory acute myeloid leukemia to test the efficacy of magrolimab.
Patients with low-risk myelodysplastic syndrome saw more durable responses and higher tolerability when taking luspatercept-aamt compared with the placebo.
Standard of care treatment was superior to the combination of ibrutinib plus venetoclax in terms of decreasing minimal residual disease for previously untreated patients with chronic lymphocytic leukemia.
The time-limited combination of ibrutinib plus chemoimmunotherapy in younger fit patients with chronic lymphocytic leukemia increased the rate of complete responses with bone marrow undetectable minimal residual disease, regardless of IGHV mutation, according to long-term follow-up data.
Patients with previously untreated chronic lymphocytic leukemia derived a better progression-free survival benefit from treatment with ibrutinib and rituximab vs fludarabine, cyclophosphamide, and rituximab.
Elderly patients treated with ibrutinib-containing regimens for chronic lymphocytic leukemia saw a progression-free survival benefit vs those who received rituximab and bendamustine.

A study presented at 2021 ASH found that costs and time spent managing adverse effects varied significantly in patients with chronic lymphocytic leukemia who were being treated with acalabrutinib, ibrutinib, and venetoclax.
Tolerable safety and durable remissions seen with ublituximab and umbralisib plus ibrutinib for patients with chronic lymphocytic leukemia who had detectable minimal residual disease after previous ibrutinib therapy.

Improvement in major molecular response rate and depth of response coupled with a favorable safety profile were noted with asciminib vs bosutinib in patients with chronic-phase chronic myeloid leukemia.
After 3 years of follow-up in the ASCEND study, progression-free survival continues to favor acalabrutinib vs investigator’s choice of therapy for relapsed chronic lymphocytic leukemia.
Patients with chronic lymphocytic leukemia experienced improved quality of life after being treated with continuous ibrutinib and rituximab, as well as frontline fludarabine, cyclophosphamide, and rituximab.
The infusion of E-Coli- and Erwinia-derived asparaginase therapies combined with chemotherapy appeared to be well tolerated with biological efficacy in patients with acute lymphoblastic leukemia under the age of 55, providing an additional option for patients for whom further asparagine treatment is contraindicated due to toxicity.
In a population of patients with chronic myeloid leukemia with resistant disease experienced promising activity following treatment with ponatinib regardless of T315I mutation status.

Jennifer A. Woyach, MD, spoke about the phase 3 AO41202 study, which investigated different ibrutinib regimens for elderly patients with chronic lymphocytic leukemia.
High rates of undetectable minimal residual disease were found in fit patients with chronic lymphocytic leukemia who were treated with venetoclax plus either obinutuzumab or ibrutinib vs chemoimmunotherapy.
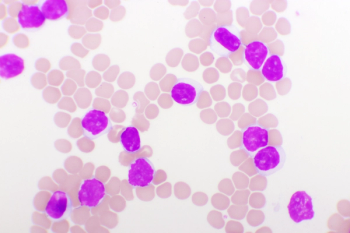
Ibrutinib and ventoclex given in the frontline setting demonstrated deeper and longer minimal residual disease for elderly and unfit patients with chronic lymphocytic leukemia.