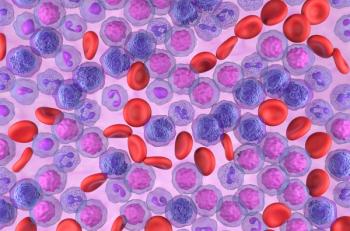
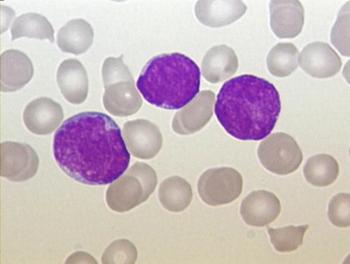
Phase 3 data show meaningful benefits with uproleselan in patients with primary refractory AML and post-transplant survival.

Your AI-Trained Oncology Knowledge Connection!

Phase 3 data show meaningful benefits with uproleselan in patients with primary refractory AML and post-transplant survival.
Zanubrutinib maintained a PFS benefit at 5 years vs benadmustine and rituximab for patients with CLL/SLL.

For patients with acute lymphoblastic leukemia and mantle cell leukemia, lymphodepletion then brexu-cel show positive efficacy and safety outcomes.
Acalabrutinib-based treatment also improves overall survival vs standard chemoimmunotherapy in the phase 3 AMPLIFY trial.
Patients aged 60 to 69 years old had comparable efficacy when treated with brexu-cel for relapsed/refractory B-cell ALL.

Olverembatinib appears effective in patients with CP-CML without T315I mutations following prior first-line tyrosine kinase inhibitor therapy.

Addressing socioeconomic barriers may help ensure that all patients with AML can benefit from potentially curative therapies.

Responses with epcoritamab were comparable across the expansion and optimization cohorts in the EPCORE CLL-1 trial.

Bulkiness of disease did not appear to impact PFS outcomes with ibrutinib plus venetoclax in the phase 2 CAPTIVATE study.
Findings from the SAVE study showed that an all-oral revumenib-based combination may improve responses in patients with acute myeloid leukemia with certain genetic alterations.
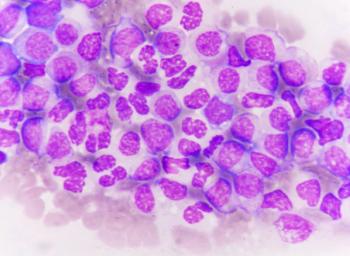
For patients with relapsed or refractory KMT2Ar acute leukemia, revumenib showed promising outcomes of overall response rate and duration of response.

Blinatumomab plus chemotherapy may represent a new treatment standard for most patients with standard-risk B-ALL, says Rachel E. Rau, MD.

Bicistronic CD19/CD22 CAR T-cell therapy had improved safety, durability, and high remission rates in pediatric patients with R/R B-ALL.

Combining olverembatinib with blinatumomab appears to produce high complete molecular remission rates in patients with newly diagnosed, Philadelphia chromosome–positive acute lymphoblastic leukemia, says Elias Jabbour, MD.
Patients with chronic lymphocytic leukemia in the ALPINE study previously treated with BTK inhibitors are likely to remain sensitive to other BTK-targeting agents, says Jennifer Brown, MD, PhD.
Pirtobrutinib produces a high rate of responses in patients with relapsed chronic lymphocytic leukemia harboring baseline BTK mutations, according to findings from the phase 1/2 BRUIN trial.
Data from the phase 3 SEQUIOA trial may support zanubrutinib as a best-in-class Bruton tyrosine kinase inhibitor in the frontline management of chronic lymphocytic leukemia.

Fixed-dose ibrutinib plus venetoclax produces limited second malignancies among patients with chronic lymphocytic leukemia, says Paolo Ghia, MD, PhD.

Treatment with lisocabtagene maraleucel in the TRANSCEND CLL 004 study raises no new safety concerns in patients with relapsed/refractory chronic lymphocytic leukemia, says Tatyana Feldman, MD.

Asciminib results in greater efficacy, safety, and tolerability compared with bosutinib in patients with chronic myeloid leukemia, according to findings from the phase 3 ASCEMBL study.

Ibrutinib plus venetoclax appears to be effective across the overall chronic lymphocytic leukemia population in the CAPTIVATE study, although progression-free survival is shorter for those with TP53 mutations.
Revumenib treatment results in durable MRD-negative remissions in pediatric and adult patients with relapsed/refractory KMT2A rearranged acute leukemia in the phase 2 Augment-101 study.
Acalabrutinib on its own or in combination with obinutuzumab increases PFS and ORR in patients with chronic lymphocytic leukemia regardless of mutation status, according to follow-up data from the ELEVATE-TN trial.

Patients with NPM1-mutated acute monocytic leukemia who are minimal residual disease negative do not appear to benefit from allogeneic stem cell transplant after chemotherapy induction, even with a FLT3 ITD co-mutation.
Treatment outcomes with obecabtagene autoleucel in patients with relapsed/refractory B-cell acute lymphoblastic leukemia appear to be better in those with lower leukemia burden at lymphodepletion in the FELIX study.
Data from the phase 1/2 BRUIN study support continuous BTK pathway inhibition as an important sequencing approach in chronic lymphocytic leukemia or small lymphocytic lymphoma, says Jennifer A. Woyach, MD.

Treatment with zanubrutinib also appears to improve overall survival compared with ibrutinib among patients with relapsed/refractory chronic lymphocytic leukemia or small lymphocytic lymphoma in the phase 3 ALPINE trial.
Treatment with venetoclax appears to be well-tolerated in patients with chronic lymphocytic leukemia or small lymphocytic lymphoma, says Nilanjan Ghosh, MD, PhD.
Results from the phase 1/2 SAVE trial demonstrated an improved objective response rate when revumenib was added to decitabine/cedazuridine, and venetoclax for patients with relapsed/refractory acute myeloid leukemia.

Patients with promyelocytic leukemia saw an improved overall survival and relapse-free survival when treated with an all-oral regimen of arsenic trioxide, all-trans retinoic acid, and ascorbic acid.