
Patients with glioblastoma who were uninsured or who had Medicaid at the time of diagnosis were more likely to be diagnosed with a larger tumor and had shorter survival times.

Your AI-Trained Oncology Knowledge Connection!


Patients with glioblastoma who were uninsured or who had Medicaid at the time of diagnosis were more likely to be diagnosed with a larger tumor and had shorter survival times.
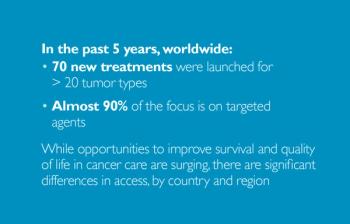
Read compelling analyses of 5-year trends and projected changes in the oncology clinical drug pipeline, selected from the IMS Institute for Healthcare Informatics’ recent “Global Oncology Trend Report.”

Are you up to date on the latest BRAF and MEK inhibitors used in melanoma? How about the most common location of metastasis in uveal melanoma? Answer these questions and more.

Ten percent of advanced cancer patients have developed delirium, but it is often missed by emergency department physicians.

Patients continue to say they want more information, so they can make informed decisions. But repeatedly, studies tell us that the patient and the family are not hearing us, not understanding us, or both.

A recent study found that radiologists differ in their interpretation of whether a woman has dense breasts based on mammography.

Acupressure, a technique derived from acupuncture, helped improve sleep and relieved chronic fatigue experienced by women treated for breast cancer.

Adding the antipsychotic drug olanzapine to a standard antiemetic regimen significantly improved prevention of nausea caused by emetogenic chemotherapy.

A new study has found an increased risk for a cancer diagnosis during the 10 years prior to and the 3 months immediately after being diagnosed with type 2 diabetes.

In this Medical News Minute, developed exclusively for Cancer Network, Dr. Bobby Lazzara discusses a study that looked at the link between air pollution and the risk of various cancers.

Can you name all of the approved melanoma agents that modulate the immune system? How about the targets and side effects associated with these treatments? Answer these questions and more.

In this video we discuss the use of concurrent immunotherapy and stereotactic radiosurgery for treatment of melanoma brain metastases.

Undergoing immunotherapy within a month of stereotactic radiosurgery resulted in an improved response to treatment for patients with melanoma brain metastases.

A randomized phase III trial found that a hypofractionated radiotherapy regimen was not superior to, but generally equivalent to a conventional radiotherapy scheme in men with localized prostate cancer.

In this Medical News Minute, developed exclusively for Cancer Network, Dr. Bobby Lazzara discusses new regulations from the FDA that subject e-cigarettes and hookahs to some of the same regulations as tobacco products.

Most metastatic cancer patients are still receiving aggressive methods of treatment near the end of life, and palliative/supportive measures are significantly underutilized.

A database analysis showed that the addition of external beam radiotherapy to ADT significantly improves overall survival in men with metastatic prostate cancer.

Do you know incidence of breast cancer in the United States? How about the proportion of breast cancer patients who are men?

In this video we discuss the use of biomarker-guided treatment in phase I trials, which can yield high response rates.

Higher than average PSA levels in middle age may be predictive of a higher risk of lethal prostate cancer later in life.

The use of hemithoracic pleural IMRT after chemotherapy could become part of a new lung-sparing therapy in patients with malignant pleural mesothelioma.

In this video we discuss a large-scale genomic analysis that found that patterns of genetic changes detected in circulating tumor DNA mirror those identified in tumor tissue biopsies.
The USPSTF has issued an updated guideline with recommendations regarding screening for colorectal cancer. A systematic review found that screening can be of “substantial net benefit.”

In this interview we discuss the direct-to-consumer advertising for nivolumab (Opdivo) for the treatment patients with advanced non-small-cell lung cancer.

Effective communication between doctors and their team is key to giving the best care to patients, and can provide stress relief in a chaotic day.

In this interview we discuss follow-up care and screening for second primary cancers in cancer survivors.

Use of hypofractionated chemoradiation prior to pancreatoduodenectomy resulted in similar resection rates and outcomes vs standard fractionation.

This management guide covers the risk factors, symptoms, diagnosis, staging, and treatment of head and neck cancers (including tumors of the oral cavity, oropharynx, hypopharynx, larynx, supraglottis, glottis, subglottis, and nasopharynx) using radiation, surgery, and medical treatment.

In this interview we discuss the management of late effects from radiotherapy in patients treated for gynecologic cancers.

This management guide of endocrine malignancies covers the risk factors, diagnosis, screening, and treatment of both thyroid and parathyroid cancers.