The European Commission approved lisocabtagene maraleucel for the treatment of certain patients with relapsed/refractory large B-cell lymphoma.

Your AI-Trained Oncology Knowledge Connection!

The European Commission approved lisocabtagene maraleucel for the treatment of certain patients with relapsed/refractory large B-cell lymphoma.

Data regarding different dosing strategies of elimusertib for advanced solid tumors with ATM alterations and other DNA damage repair gene defects display early efficacy of the therapy.
Biomarker analysis and studies of pharmacokinetics, pharmacodynamics, and T-cell composition show certain T-cell characteristics are linked with outcomes and toxicity with axicabtagene ciloleucel in large B-cell lymphoma.
Investigators of a phase 1/2 trial observed positive response outcomes with expanded natural killer cells plus AMF13 in patients with heavily pretreated lymphoma.

Data presented from the 4-year follow-up to the phase 3 KEYNOTE-042 trial display continuous survival benefit of pembrolizumab vs chemotherapy in Chinese patients with untreated non–small cell lung cancer.

Early findings from the phase 1/2a TEM-GBM study presented at the 2022 AACR Annual Meeting displayed potential of temferon to affect the tumor microenvironment of glioblastoma.

Serplulimab, which has been granted orphan drug designation by the FDA, is being considered as a treatment for patients with small cell lung cancer.

Although patients with endometrial cancer who had histologically confirmed endometriosis/adenomyosis achieved better overall survival than those without, the benefit was linked to stage, grade, age, and histological subtype.

Based on results from the EPIK-P1 trial, the FDA has granted accelerated approval to alpelisib for PIK3CA-related overgrowth spectrum.
Frederick Lock, MD, spoke about the approval of axicabtagene ciloleucel and how it’s beneficial for patients with large B-cell lymphoma who were treated with frontline chemoimmunotherapy.
Data from a phase 1/2 trial examining nivolumab plus a PD-L1/IDO peptide vaccine indicates early activity in patients with metastatic melanoma, according to results from the 2022 AACR Annual Meeting.

Black patients were reported to be significantly less likely to receive standard of care surgical treatment for cancer of the gastrointestinal tract compared with White patients.
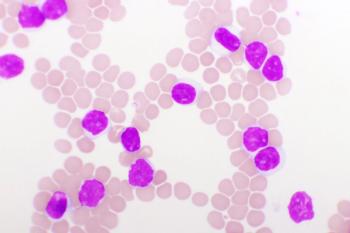
Longer and more durable remissions were identified with the addition of CART-19 to ibrutinib for patients with chronic lymphocytic leukemia.

In an interview with ONCOLOGY®, Elizabeth Travers, PharmD, BCOP, offers a comprehensive review of real-world treatment considerations of asciminib as therapy for patients with chronic myeloid leukemia.

John Kirkwood, MD, PhD, discussed considerations for treating patients with melanoma using immunotherapy and how to properly monitor responses.
At SGO 2022, Jyoti S. Mayadev, MD presented results of the NRG-GY017 trial of atezolizumab as either an immune primer or with chemoradiation for certain patients with locally advanced cervical cancer.

Patients with HER2-positive apocrine carcinoma of the breast are less likely to have an aggressive phenotype and are more likely to have favorable outcomes, even though the group has a lower rate of estrogen and progesterone receptor positivity.
Updated data from a pivotal trial that led to the approval of zanubrutinib for the treatment of patients with relapsed or refractory mantle cell lymphoma appears to highlight persistent benefit.

At the 15th Annual Interdisciplinary Prostate Cancer Congress® and Other Genitourinary Malignancies, Peter Humphrey, MD, PhD, spoke about how the conference catered to the multidisciplinary audience, and what he learned from that.
Anjali Y. Hari, MD, speaks to the rationale for examining hyperthermic intraperitoneal chemotherapy in a population of frail and non-frail patients with ovarian cancer.
Investigators spoke to the disparities that are present in multiple myeloma and possible causes such as socioeconomic factors.
The phase 1/2a TakeAim Leukemia trial assessing emavusertib alone or with azacitidine or venetoclax in relapsed/refractory acute myeloid leukemia or high-risk myelodysplastic syndrome has been placed on a partial clinical hold by the FDA.

In a discussion with CancerNetwork®, Ursula A. Matulonis, MD, describes the potential of mirvetuximab soravtansine (IMGN853) as a treatment for patients with folate receptor α (FRα)–high platinum-resistant ovarian cancer.

Ira Winer, MD, PhD, FACOG, spoke about patients with pretreated platinum-resistant ovarian cancer treated with nemvaleukin alfa plus pembrolizumab in the phase 1/2 ARTISTRY-1 trial.
In an interview with CancerNetwork®, Melissa Hardesty, MD, discusses how maintenance niraparib and bevacizumab following frontline platinum-based chemotherapy and bevacizumab yielded promising results in patients with advanced ovarian cancer.
Based on results from a phase 1 trial, the FDA has granted fast track designation to PRGN-3006 UltraCAR-Tin relapsed/refractory acute myeloid leukemia.
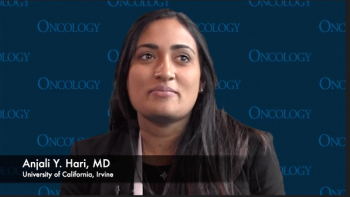
Anjali Hari, MD, discusses survival and safety outcomes with hyperthermic intraperitoneal chemotherapy in frail and non-frail patients with ovarian cancer.

In a poster presentation from Society of Gynecologic Oncology 2022 Annual Meeting, investigators led by Cara Mathews, MD, aimed to determine the benefit of dostarlimab vs standard-of-care doxorubicin for advanced recurrent endometrial cancer.

A biologics license application for omburtamab was resubmitted following a refusal to file letter in 2020 for pediatric patients with central nervous system/leptomeningeal metastatic from neuroblastoma.
Pediatric patients with high allelic ratio FLT3/ITD–positive acute myeloid leukemia may benefit from treatment with sorafenib plus chemotherapy.