
Future biomarker analysis will include correlation of efficacy with SLFN11 expression and with markers of DNA damage repair.

Your AI-Trained Oncology Knowledge Connection!


Future biomarker analysis will include correlation of efficacy with SLFN11 expression and with markers of DNA damage repair.

Gary Steinberg, MD, highlights the FDA approval of the gemcitabine intravesical system and what this means for patients with BCG-unresponsive NMIBC.

The test may help identify patients with microsatellite instability-high colorectal cancer who benefit from nivolumab therapy alone or with ipilimumab.

Data from a phase 1/2a trial showed that plixorafenib-based care achieved a median PFS of 63.9 months in patients with BRAF-altered thyroid cancers.

Ongoing studies in kidney cancer aim to explore determinants of immune-related adverse effects and strategies for mitigating them.

Data from the IDeate-Lung01 trial support the potential role that ifinatamab deruxtecan may play in the management of extensive-stage small cell lung cancer.

Findings from a phase 1 trial and the REJOICE-Ovarian01 trials supported the FDA’s decision to grant the designation to R-DXd in those with gynecologic cancers.

Machine learning–based approaches may play a role in further understanding of how somatic alterations influence responses or resistance to therapy.

The decision from the Ministry of Health, Labour and Welfare was supported by phase 3 LUNAR trial results showing an OS benefit with Optune Lua in NSCLC.

Experts detailed key advances in myelofibrosis, multiple myeloma, and lymphoma at the Society of Hematologic Oncology 2025 Annual Meeting.

Data from a first-in-disease trial assessing a personalized cancer vaccine in RCC require validation at a larger level, according to David Braun, MD, PhD.

Ateganosine plus cemiplimab was well tolerated in patients with heavily pretreated advanced NSCLC, with most adverse effects grades 1/2 in severity.

Findings from the 2025 World Conference on Lung Cancer reflected key updates in the management of NSCLC, SCLC, and other lung cancer types.

All efficacy-evaluable patients with ES-SCLC treated with surufatinib, durvalumab, etoposide, and chemotherapy responded to treatment.

A group of community and academic oncologists exchanged ideas on optimizing therapy across different prostate, kidney, and bladder cancer populations.

Experts discuss considerations for improving the care of patients with prostate, kidney, and bladder cancer in community-based practices at World GU 2025.
Full overall survival results with amivantamab plus lazertinib from the Asia cohort of the MARIPOSA trial will be shared at a future medical conference.

No new safety signals were identified with subcutaneous amivantamab in EGFR-mutant NSCLC, and infusion reactions were reduced vs the IV formulation.

Ziftomenib yielded a median overall survival of 16.4 months in responders with NPM1-mutant AML who received ziftomenib in the phase 1b/2 KOMET-001 trial.

Experts highlight methods for optimally treating patients with genitourinary cancers harboring variant histologies at World GU 2025.

At World GU 2025, experts discussed forming treatment strategies for patients with variant histologies across prostate, bladder, and kidney cancer.

After failing to record any objective responses in 9 patients with relapsed/refractory ES-SCLC, the phase 2 trial was terminated early.
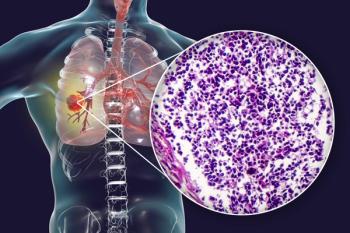
Results from the DeLLphi-303 trial showed sustained efficacy and safety with tarlatamab plus anti–PD-1 treatment for patients with extensive-stage SCLC.
![We found that patients who are [complete remission] MRD-negative, and PET/CT negative year after year for 5 years do not have to be maintained.](https://cdn.sanity.io/images/0vv8moc6/cancernetwork/a0c5316b5733cfe8ccceb396476faf0cea2f2e46-320x410.png?w=350&fit=crop&auto=format)
According to Sundar Jagannath, MBBS, the cure for multiple myeloma was observed in patients who were cancer free for 5 years without maintenance therapy.
The FDA has assigned a Prescription Drug User Fee Act date of July 11, 2026, for relacorilant as a treatment for platinum-resistant ovarian cancer.

Rezatapopt achieved an ORR of 33% in all patients, and an ORR of 43% in patients with ovarian cancer, with 1 confirmed complete response.

The FDA approved selumetinib as treatment for pediatric neurofibromatosis type 1, expanding options for young patients with inoperable plexiform neurofibromas.

Rates of grade 3 or 4 AEs with durvalumab were similar across subgroups, with serious AEs more frequent in patients 70 years or older with ES-SCLC.

In patients who refuse or are ineligible for radical cystectomy, the gemcitabine intravesical system may be given after unsuccessful BCG treatment.

When compared with observation, adjuvant crizotinib did not improve disease-free survival or overall survival in ALK-positive NSCLC.