Antibody-drug conjugates like Rina-S may be able to salvage some of the responses that are often lost in the later lines of treatment, according to Elizabeth Lee, MD.

Your AI-Trained Oncology Knowledge Connection!

Antibody-drug conjugates like Rina-S may be able to salvage some of the responses that are often lost in the later lines of treatment, according to Elizabeth Lee, MD.

Modakafusp alfa induced the upregulation of the type 1 interferon gene signature score, and increased CD38 receptor density in CD-38–positive cells.
No grade 3 or higher treatment-related adverse effects or deaths were reported among those with non-muscle invasive bladder cancer in the BOND-003 trial.

Recipients of hematopoietic stem cell transplantation may benefit from psychosocial interventions and supportive care following their procedure.

Increased incidence and mortality rates for cervical cancer among rural women in the US may result from barriers to access to care.
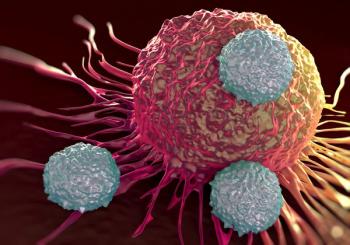
“There is, potentially, a role for Rina-S or other novel ADCs targeting different epitopes on the cancer cell surface,” Elizabeth Lee, MD, stated.
In patients who were pretreated and treatment naïve with RET fusion-positive NSCLC, selpercatinib yielded an ORR of 61.5% and 82.6%, respectively.

Results from the RAINIER trial showed that mipletamig, venetoclax, and azacitidine achieved a complete remission rate of 90% in patients with AML.
The adverse effect profile was similar among patients with prostate cancer using NeuroSAFE-assisted RARP vs standard RARP.

Clara Bodelon, PhD, MS, discussed her recently published study which found that the greatest physical health declines in patients who survived breast cancer stemmed from chemotherapy.

Experts from Washington University in St. Louis discuss prior data and strategies for mitigating toxicities like CRS associated with tarlatamab in SCLC.

Nivolumab-based therapies showed improved efficacy vs chemotherapy in hypermutated and Epstein-Barr virus–positive gastroesophageal tumors.
Updated findings from the CENTAURUS study may support the use of daratumumab monotherapy in those with intermediate- or high-risk smoldering myeloma.
“As a field, we’re trying to push hard to make [radiation] patient-centered, and because of that, the field is the future of the field is pretty bright,” James B. Yu, MD, MHS, FASTRO, stated.

Prolonging systemic therapy in patients with gastric or gastroesophageal junction cancers may offer better outcomes than radiation therapy.
James B. Yu, MD, MHS, FASTRO, believes that 2 of the most intriguing and growing areas of radiation oncology are reirradiation of the prostate and bladder chemoradiation.

In the phase 2 EPOCI1802 trial, atezolizumab monotherapy elicited a cCR rate of 42.1%, an ORR of 65.8%, and a 12-month OS rate of 65.8% in advanced ESCC.

Most adverse effects observed in combination therapies for gastric cancers are associated with chemotherapy, according to Yelena Y. Janjigian, MD.
Phase 2 data may support atezolizumab plus chemotherapy as a treatment option in advanced or recurrent thymic carcinoma.
“The idea is that the patients are informed of the long-term consequences [of the treatments] so they can have some [input in] decision making,” Clara Bodelon, PhD, MS, stated.
The complete response letter for camrelizumab/rivoceranib for patients with advanced HCC did not specify what deficiencies regulators found.

The new drug application for TLX007-CDx has been approved by the FDA for patients with prostate cancer.
Elotuzumab in combination with pomalidomide, bortezomib, and dexamethasone was well tolerated in patients with relapsed/refractory multiple myeloma.

Christina Henson, MD, discusses recent phase 3 trial results comparing durvalumab to cetuximab in head and neck cancer, and why the trial was stopped early.

Select comorbidities, ECOG status, and the receipt of radiation were among the differences between a real-world cohort and the RUBY trial population.
Timely guideline-concordant care may mitigate racial and ethnic disparities in overall survival among patients with inflammatory breast cancer.
Azer-cel elicited strong and durable responses in patients with heavily pretreated relapsed/refractory DLBCL in a phase 1b trial.

Evaluation of the 1-year overall survival data in the phase 3 ARES trial assessing MaaT013 in GVHD is expected to occur Q4 2025.

Real-world atezolizumab plus chemotherapy data demonstrated similar efficacy compared with what the phase 3 IMpower133 trial showed.

Future work may need to assess whether extended hospital stays improve surgical care outcomes during disasters, according to one of the study authors.