- ONCOLOGY Vol 12 No 4
- Volume 12
- Issue 4
Cancer and Male Factor Infertility
With the increasing success of multimodality anticancer therapy, most men of reproductive age will survive their malignancy. Reproductive function is a principal concern of these men. Health-care providers are shifting the
Cancer and Male Factor Infertility: It May Only Take One Sperm, But Make Sure Its There
Advances in the treatment of malignancies have led to new problemsside effects and complications of radiation and chemotherapy. Foremost on both physicians and patients minds is the struggle for survival, as it should be, but part of self-preservation is the drive by members of most species to pass on their seed. Thus, a paradox develops between delivery of new, more powerful ways to treat malignancies and the simultaneous destruction of innocent bystanders: sperm and eggs.
This article by Costabile and Spevak nicely reviews the pre-treatment abnormalities in male reproductive function, the gonadotoxic effects of cancer treatments, and the recovery of testicular function after treatment. The authors also review methods of altering treatment protocols after therapy to maximize reproductive potential and to treat cancer patients who are infertile. This is clearly an important topic for everyone who treats men with cancer.
Take-Home Message
Assisted reproductive techniques have come of age with the advent of intracytoplasmic sperm injection. In the past, more sperm was better. Lots of sperm were generally needed for conception, whether it be through intercourse, intrauterine insemination, or in vitro fertilization. With intracyotoplasmic sperm injection, only one sperm per egg is needed. Thus, the adage, it only takes one sperm, is now true.
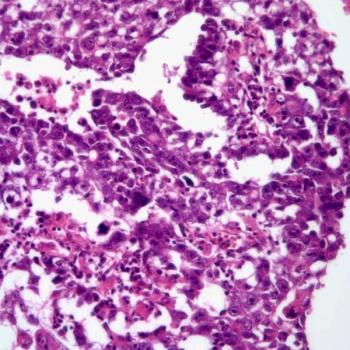
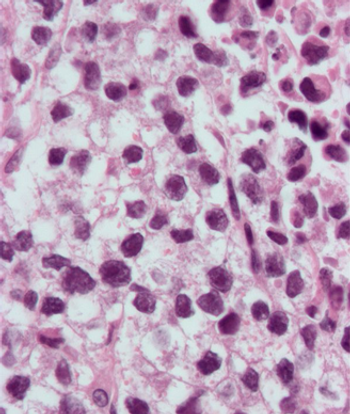
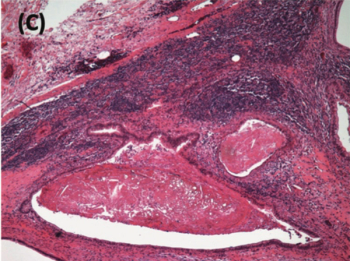
Witt and colleagues gave this concept support with their 1995 report of the first testicular sperm extraction in the United States.[1] A 32-year-old man with congenital bilateral absence of the vas deferens had the procedure, followed by in vitro fertilization with intracytoplasmic sperm injection and the delivery of a healthy baby boy. The technology for testicular sperm extraction has progressed to the point that we are able to obtain testicular sperm from men with azoospermia even if the testicles show maturation arrest or Sertoli cells only (ie, no apparent germ cells by pathologic diagnosis). What an advance for the oncology patient who desperately wants children but has no sperm in his ejaculate because of radiation or chemotherapy!
A man with only a few sperm within his testicle can have that sperm harvested by TESE, injected into eggs by intracytoplasmic sperm injection, and in approximately 25% of cases achieve a pregnancy by IVF that is followed by a live birth. Intracytoplasmic sperm injection is a major development for the male oncology patient who wants children and is the most important message of this timely review.
The Forgotten Message
Fertility has taken a back seat for so long in the treatment of the cancer patient, that it is often completely forgotten. I was recently approached by a woman who had a male relative who had been treated for testicular cancer when he was 18 years old. She said that he was offered the opportunity to have his sperm frozen prior to receiving chemotherapy but did not do so. Not surprisingly, fertility was not uppermost in the mind of this 18-year-old male with cancerstaying alive was. Now he is 27 years old, cured of cancer, and very upset that he has no frozen sperm and his testis biopsy shows no sperm.
As physicians, when do we offer chemotherapy or radiation therapy? We dont offer, we usually direct the patient to what is best for him or her. Likewise, we should direct all males who can give a sample, and are not beyond their reproductive years, to cryopreserve their sperm. This should happen routinely, and yet anecdotale evidence suggests that it happens rarely. It should also happen early, right after diagnosis and before treatment. Yet, if the offer to cryopreserve sperm is made, it is often made the day before treatmenthardly enough time to collect adequate samples. Three to five specimens are usually adequate. It costs about $500 to $1,000 to freeze three specimens and about $200 per year for storage. Insurance coverage for cryopreserv- ation of sperm varies tremendously. These facts and the importance of cryopreservation of sperm need to be an integral part of medical and radiation oncologists' discussions with patients about treatment.
At the Crossroads
When the lithotriptor that so effectively treated kidney stones was invented, much of the drive to understand why some people form kidney stones disappeared. Although the lithotripter treated the disease, we still did not have a cure for kidney stones. Likewise, with cryopreservation of sperm, in vitro fertilization, and intracytoplasmic sperm injec-
tion, there may be little impetus to research less toxic protocols for delivering chemotherapeutic drugs or radiation or ways to protect the testis. Although in vitro fertilization with intracytoplasmic sperm injection is a significant boon to the cancer patient who was wise enough to cryopreserve his sperm or has some sperm after therapy, it costs a fair amount of money (approximately $10,000 per in vitro fertilization cycle). Its success rate, although good, is not perfect, with about a 25% take-home baby rate per cycle.
Given a choice, most couples would rather conceive through intercourse than in vitro fertilization. So now is the time to be thankful for this wondrous technology that can help to create life after near death. However, it is also the time to continue our search for better protocols to treat cancer and better ways to protect the testes. Until these methods that preserve fertility in the cancer patient are perfected, do as we do in Minnesota: freeze, freeze, freeze (the sperm)!
References:
1. Witt MA, Elsner C, Kort HI, et al: A live birth from intracytoplasmic injection of a spermatozoon retrieved from testicular parenchyma. J Urol 154:1136-1137, 1995.
Articles in this issue
almost 28 years ago
Prevalence of Substance Abuse Disorders in Cancer Patientsalmost 28 years ago
Public Access to ONS Online Cancer Information Service Now Availablealmost 28 years ago
Finnish Study Suggests Vitamin E Prevents Prostate Canceralmost 28 years ago
Gene Linked to Breast, Ovarian, and Uterine Cancersalmost 28 years ago
ONS Issues Position Statement on Short-Stay Surgery for Breast Canceralmost 28 years ago
Scientists Shed Light on Anticancer Effects of SoybeansNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.