Gastrointestinal Cancer
Latest News
Latest Videos

Podcasts
CME Content
More News

Although findings did not show differences in eating restrictions 1 month following gastrectomy, the mobile intervention may help with symptom management.

The approval of durvalumab plus FLOT for patients with resectable gastric/GEJ cancer cements itself as a new standard of care in the space.

Clinicians who are experienced with immunotherapy, like durvalumab, can easily identify and manage AEs associated with treatment for gastric/GEJ cancer.

Based on results from the MATTERHORN study of durvalumab/FLOT in gastric/GEJ cancers, the regimen should be considered a new SOC.

Yelena Y. Janjigian, MD, provides the background of the MATTERHORN trial, showcasing the importance of durvalumab plus FLOT in gastric/GEJ cancers.

The addition of pelareorep to standard-of-care therapy in patients with KRAS-mutated microsatellite-stable CRC exhibited an ORR of 33%.

A panel of experts gathered to discuss results from the MATTERHORN trial assessing durvalumab plus FLOT in gastric/GEJ cancer.

The COMPASSION-37 study is the second international registrational study for cadonilimab following an ongoing trial in hepatocellular carcinoma.

The incidence and severity of AEs with eryaspase/chemotherapy was generally consistent with previous reports of chemotherapy alone in advanced PDAC.
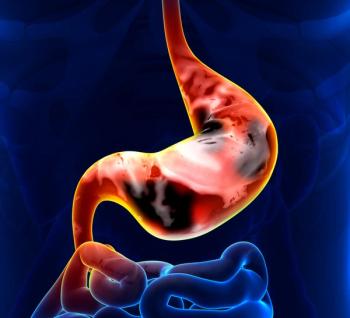
Qualified surgeons may offer laparoscopic distal gastrectomy as an alternative to open distal gastrectomy among those with clinical T4a gastric cancer.

Findings from the HERIZON-BTC-01 trial support HER2 as a valid therapeutic target in biliary tract cancer.

Results from MATTERHORN showed durvalumab plus FLOT improved EFS and OS compared with placebo plus FLOT in patients with gastric/GEJ cancers.

Results from the NAPOLI 3 trial found NALIRIFOX is a viable option for first-line treatment of metastatic pancreatic adenocarcinoma.

The safety profile of zanidatamab plus chemotherapy with or without tislelizumab was consistent with the known profiles of each individual agent.
Receiving treatment at an academic center may improve the probability of receiving subsequent curative care among those with hepatocellular carcinoma.

Results from the phase 3 COMPETE trial demonstrated that 177Lu-edotreotide improved PFS and ORR compared with everolimus in patients with GEP-NETs.
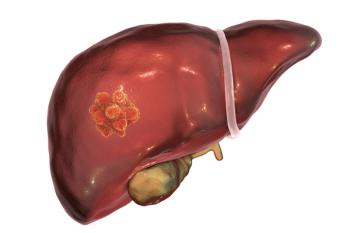
DFS rates at 2 years were improved with cemiplimab plus SBRT vs cemiplimab alone in patients with resectable hepatocellular carcinoma.

Phase 2 data show consistent overall immunotherapy immunogenicity with ELI-002 7P in those with KRAS-mutated pancreatic ductal adenocarcinoma.

Results from the PEAK trial showed increased PFS in the bezuclastinib plus sunitinib arm vs sunitinib alone for patients with GIST.

Data from the phase 2 INTERACT-ION trial support further investigation of the potential synergistic effect of ezabenlimab plus adaptive chemoradiotherapy.
Micheal C. Soulen, MD, spoke about his presentation on the CapTemY90 trial at the 2025 NANETS Multidisciplinary NET Medical Symposium.

Considering historical trends of underpowered data in NET surgical studies, CUTNETs established a collaboration of surgical teams to better power research.

A shorter course of radiotherapy may provide similar oncological outcomes as long-course treatment for older patients with locally advanced rectal cancer.
Three GI cancer medical oncologists discuss the most significant abstracts in GI cancers from the 2025 ESMO Congress.

The safety profile of lenvatinib/pembrolizumab plus TACE among patients with unresectable HCC was consistent with previously reported studies.